
Search
Statistics
We have 222 registered usersThe newest registered user is raheelmemon
Our users have posted a total of 1140 messages in 613 subjects
If you are seeing this, you have attempted to link to the UpToDate widget but are experiencing a problem. Please visit UpToDate for more information.
PRITE High Yield Topic Discussion Thread
4 posters
FORUM FOR PSYCHIATRY RESIDENTS :: Psychiatry :: Psychiatry-Neurology-Psychology discussion :: Psychiatry In Depth
Page 3 of 4
Page 3 of 4 •  1, 2, 3, 4
1, 2, 3, 4 
 PRITE High Yield Topic Discussion Thread
PRITE High Yield Topic Discussion Thread
First topic message reminder :
Hi Friends.
This thread is dedicated to PRITE (Psychiatry Resident-In-Training Examination) Preparation.
Please contribute important high yield topics and notes here.
INDEX:
Page 1:
• Typical Antipsychotics
• Borderline Personality Disorder
• Schizophrenia
• Dopaminergic Pathway Functions & Effect of Antipsychotics
• Sigmund Freud’s Structural Model- The id, ego, and superego
• Major depression with Atypical features
• Akathisia treatment
• Rabbit Syndrome
• Risperidone vs Clozapine
Page 2:
• Cluster A Personality disorder- differential diagnosis
• Cluster B Personality disorder- differential diagnosis
• Cluster C Personality disorder- differential diagnosis
• Personality disorder in toto (HY Facts)
• Frontotemporal dementia Vs Alzheimer’s dementia
• Autoreceptors Vs Heteroreceptors
• Visual Pathway And Associated Visual Defects
• Myasthenia Gravis
• Jean Piaget's Cognitive Development Stages
• Normal Aging- Facts
• Erikson's Stages of Psychosocial Development
• Cognitive Theory for depression Management
Page 3:
• Interpersonal Therapy (IPT)
• Valproate
• Childhood Onset Schizophrenia
• Recommendations for monitoring adults on atypical antipsychotics
• Pediatric Depression- Which SSRI is Superior
• Neuroleptic Malignant Syndrome
• Hispanic culture-bound syndromes
• Elevated Clozapine Levels
• Pervasive Developmental Disorder Not Otherwise Specified (Including Atypical Autism)
• Diagnostic criteria for Attention-Deficit/Hyperactivity Disorder
• Diagnostic criteria for Gender Identity Disorder
• Freud's Topographical Model
• HIV Dementia/Toxoplasmosis/CNS Lymphoma/Cryptococcal Meningitis/PML
• Gait Abnormalities
Page 4:
• Trigeminal neuralgia Vs Post Herpetic Neuralgia
• Carbon Monoxide Toxicity: Brain MRI Findings
• Lumbar & Sacral Nerve Root Compromise
• Classic Conditioning Vs Operant Conditioning
• Observational Study Design: Case control Vs Cohort
• Alexia/Apraxia/Agnosia/Akinesia/Aphasia
• Adjustment Disorders Vs Acute Stress Disorder
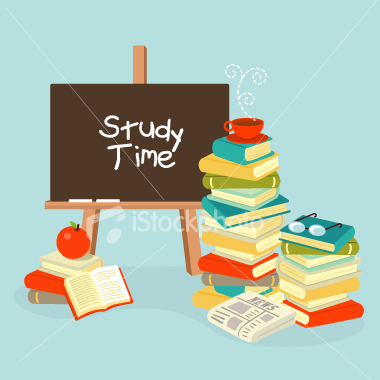
• SNRIs: Venlafaxine Vs Duloxetine
• DSM IV Criteria for Manic Episode
• Bipolar Disorder: 15 Minutes CORE Psychiatric Evaluation- 4 Decision Points
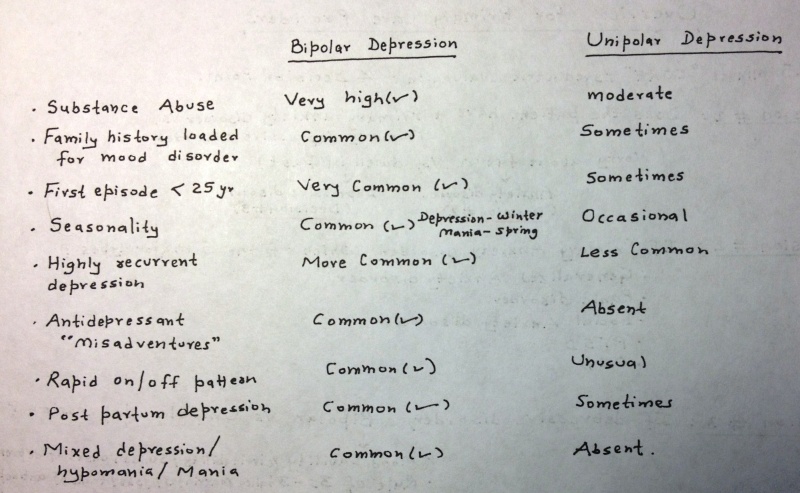
• Bipolar Depression Vs Unipolar Depression
• Difference Between Classical Conditioning & Extinction
• "Neurology" Questions/HY Facts for PRITE (Post 1 & 2)
Page 5:
• Catatonia
• CVA
• "Delirium" & "Dementia"
• Seizure
• Obsessive-compulsive disorders
• Role of Ziprasidone in combination therapy for Bipolar maintenance
• Recognition of GAD in Primary Care Setting
• Social Anxiety Disorder
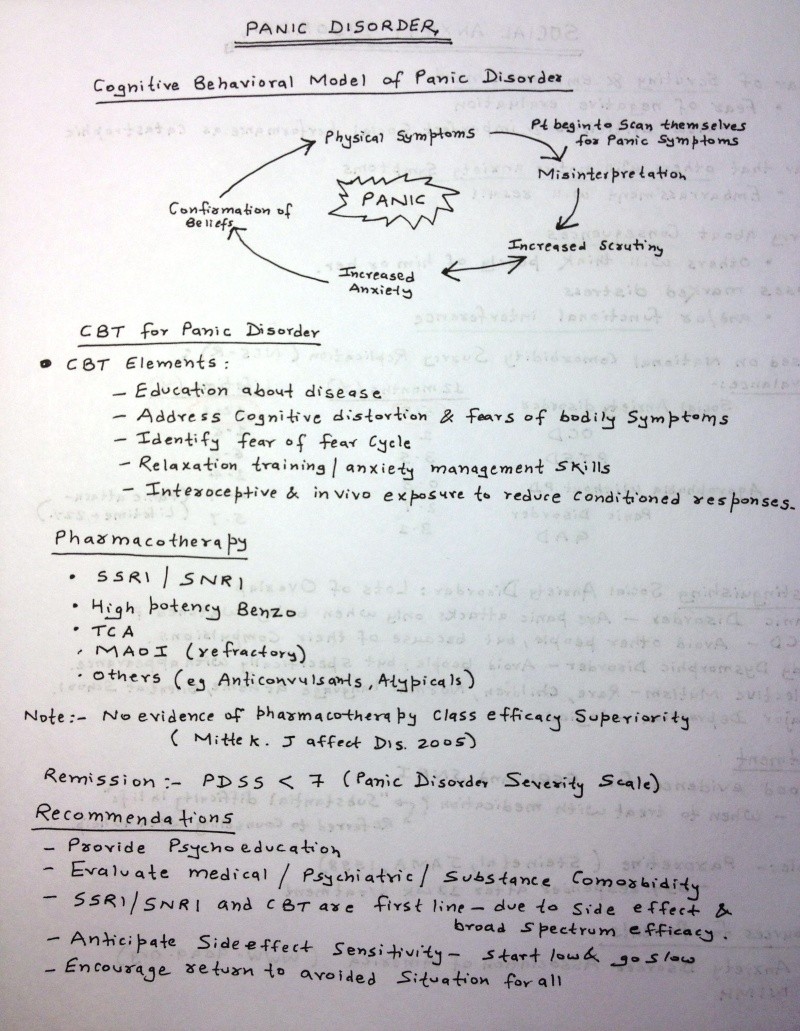
• Panic Disorder
• ADHD (Recent Facts)
• Basics of Nor-Epinephrine, Dopamine & Seretonin Neurons.
• Hyperprolactinaemia With Antipsychotics
• Idiopathic Parkinson Ds Vs Other Parkinsonian Syndrome
• Pathophysiology of Neuroleptic Malignant Syndrome (NMS)
Page 6:
• Treatment of Juvenile Myoclonic Epilepsy
• Borderline Personality Disorder- What Questions to Ask?
• Transient Global Amnesia- Facts.
• Effective Dose for Antipsychotics- ED50 & Near-Maximal ED
• Fatal Familial Insomnia
• Medications for Alcohol Dependence
• Serotonin Toxicity- Diagnostic Criteria
• Alexithymia
• AACAP Practice Parameters for Bipolar Disorder in Children
• Progressive Supranuclear Palsy Vs Parkinson's disease
• Treatment of Depression with Atypical Features
• Types of Aphasia
• The Social Learning Theory of Julian B. Rotter
***** Updated Daily *****
Regards
Administrator
Hi Friends.
This thread is dedicated to PRITE (Psychiatry Resident-In-Training Examination) Preparation.
Please contribute important high yield topics and notes here.

INDEX:
Page 1:
• Typical Antipsychotics
• Borderline Personality Disorder
• Schizophrenia
• Dopaminergic Pathway Functions & Effect of Antipsychotics
• Sigmund Freud’s Structural Model- The id, ego, and superego
• Major depression with Atypical features
• Akathisia treatment
• Rabbit Syndrome
• Risperidone vs Clozapine
Page 2:
• Cluster A Personality disorder- differential diagnosis
• Cluster B Personality disorder- differential diagnosis
• Cluster C Personality disorder- differential diagnosis
• Personality disorder in toto (HY Facts)
• Frontotemporal dementia Vs Alzheimer’s dementia
• Autoreceptors Vs Heteroreceptors
• Visual Pathway And Associated Visual Defects
• Myasthenia Gravis
• Jean Piaget's Cognitive Development Stages
• Normal Aging- Facts
• Erikson's Stages of Psychosocial Development
• Cognitive Theory for depression Management
Page 3:
• Interpersonal Therapy (IPT)
• Valproate
• Childhood Onset Schizophrenia
• Recommendations for monitoring adults on atypical antipsychotics
• Pediatric Depression- Which SSRI is Superior
• Neuroleptic Malignant Syndrome
• Hispanic culture-bound syndromes
• Elevated Clozapine Levels
• Pervasive Developmental Disorder Not Otherwise Specified (Including Atypical Autism)
• Diagnostic criteria for Attention-Deficit/Hyperactivity Disorder
• Diagnostic criteria for Gender Identity Disorder
• Freud's Topographical Model
• HIV Dementia/Toxoplasmosis/CNS Lymphoma/Cryptococcal Meningitis/PML
• Gait Abnormalities
Page 4:
• Trigeminal neuralgia Vs Post Herpetic Neuralgia
• Carbon Monoxide Toxicity: Brain MRI Findings
• Lumbar & Sacral Nerve Root Compromise
• Classic Conditioning Vs Operant Conditioning
• Observational Study Design: Case control Vs Cohort
• Alexia/Apraxia/Agnosia/Akinesia/Aphasia
• Adjustment Disorders Vs Acute Stress Disorder
• SNRIs: Venlafaxine Vs Duloxetine
• DSM IV Criteria for Manic Episode
• Bipolar Disorder: 15 Minutes CORE Psychiatric Evaluation- 4 Decision Points
• Bipolar Depression Vs Unipolar Depression
• Difference Between Classical Conditioning & Extinction
• "Neurology" Questions/HY Facts for PRITE (Post 1 & 2)
Page 5:
• Catatonia
• CVA
• "Delirium" & "Dementia"
• Seizure
• Obsessive-compulsive disorders
• Role of Ziprasidone in combination therapy for Bipolar maintenance
• Recognition of GAD in Primary Care Setting
• Social Anxiety Disorder
• Panic Disorder
• ADHD (Recent Facts)
• Basics of Nor-Epinephrine, Dopamine & Seretonin Neurons.
• Hyperprolactinaemia With Antipsychotics
• Idiopathic Parkinson Ds Vs Other Parkinsonian Syndrome
• Pathophysiology of Neuroleptic Malignant Syndrome (NMS)
Page 6:
• Treatment of Juvenile Myoclonic Epilepsy
• Borderline Personality Disorder- What Questions to Ask?
• Transient Global Amnesia- Facts.
• Effective Dose for Antipsychotics- ED50 & Near-Maximal ED
• Fatal Familial Insomnia
• Medications for Alcohol Dependence
• Serotonin Toxicity- Diagnostic Criteria
• Alexithymia
• AACAP Practice Parameters for Bipolar Disorder in Children
• Progressive Supranuclear Palsy Vs Parkinson's disease
• Treatment of Depression with Atypical Features
• Types of Aphasia
• The Social Learning Theory of Julian B. Rotter
***** Updated Daily *****
Regards
Administrator
Last edited by Admin on Sun Nov 24, 2013 7:29 pm; edited 67 times in total
 Re: PRITE High Yield Topic Discussion Thread
Re: PRITE High Yield Topic Discussion Thread
Alexia: patient lose the ability to read. It is also called word blindness, text blindness or visual aphasia.
Apraxia: loss of the ability to execute or carry out learned purposeful movements, despite having the desire and the physical ability to perform the movements
Agnosia: loss of ability to recognize objects, persons, sounds, shapes, or smells while the specific sense is not defective nor is there any significant memory loss
Akinesia: inability to initiate movement
Aphasia: impairment of language ability
 Re: PRITE High Yield Topic Discussion Thread
Re: PRITE High Yield Topic Discussion Thread
Adjustment Disorders Vs Acute Stress Disorder
Diagnostic criteria for Adjustment Disorders
A. The development of emotional or behavioral symptoms in response to an identifiable stressor(s) occurring within 3 months of the onset of the stressor(s).
B. These symptoms or behaviors are clinically significant as evidenced by either of the following:
1. marked distress that is in excess of what would be expected from exposure to the stressor
2. significant impairment in social or occupational (academic) functioning
C. The stress-related disturbance does not meet the criteria for another specific Axis I disorder and is not merely an exacerbation of a preexisting Axis I or Axis II disorder.
D. The symptoms do not represent Bereavement.
E. Once the stressor (or its consequences) has terminated, the symptoms do not persist for more than an additional 6 months.
Specify if:
- Acute: if the disturbance lasts less than 6 months
- Chronic: if the disturbance lasts for 6 months or longer
Adjustment Disorders are coded based on the subtype, which is selected according to the predominant symptoms. The specific stressor(s) can be specified on Axis IV.
309.0 With Depressed Mood
309.24 With Anxiety
309.28 With Mixed Anxiety and Depressed Mood
309.3 With Disturbance of Conduct
309.4 With Mixed Disturbance of Emotions and Conduct
309.9 Unspecified
Diagnostic criteria for 308.3 Acute Stress Disorder
A. The person has been exposed to a traumatic event in which both of the following were present:
1. the person experienced, witnessed, or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others
2. the person's response involved intense fear, helplessness, or horror
B. Either while experiencing or after experiencing the distressing event, the individual has three (or more) of the following dissociative symptoms:
1. a subjective sense of numbing, detachment, or absence of emotional responsiveness
2. a reduction in awareness of his or her surroundings (e.g., "being in a daze")
3. derealization
4. depersonalization
5. dissociative amnesia (i.e., inability to recall an important aspect of the trauma)
C. The traumatic event is persistently reexperienced in at least one of the following ways: recurrent images, thoughts, dreams, illusions, flashback episodes, or a sense of reliving the experience; or distress on exposure to reminders of the traumatic event.
D. Marked avoidance of stimuli that arouse recollections of the trauma (e.g., thoughts, feelings, conversations, activities, places, people).
E. Marked symptoms of anxiety or increased arousal (e.g., difficulty sleeping, irritability, poor concentration, hypervigilance, exaggerated startle response, motor restlessness).
F. The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning or impairs the individual's ability to pursue some necessary task, such as obtaining necessary assistance or mobilizing personal resources by telling family members about the traumatic experience.
G. The disturbance lasts for a minimum of 2 days and a maximum of 4 weeks and occurs within 4 weeks of the traumatic event.
H. The disturbance is not due to the direct physiological effects of a substance (e.g., a drug of abuse, a medication) or a general medical condition, is not better accounted for by Brief Psychotic Disorder, and is not merely an exacerbation of a preexisting Axis I or Axis II disorder.
 Re: PRITE High Yield Topic Discussion Thread
Re: PRITE High Yield Topic Discussion Thread
Bipolar Disorder: 15 Minutes CORE Psychiatric Evaluation- 4 Decision Points


 Re: PRITE High Yield Topic Discussion Thread
Re: PRITE High Yield Topic Discussion Thread
Difference Between Classical Conditioning & Extinction
Classical Conditioning:
Repeated pairing of Neutral Stimulus + Emotionally Salient Stimulus --> Eventually Neutral Stimulus evokes Emotional Response
Extinction:
Repeated pairing of Neutral Stimulus + ABSENCE of Emotional Stimulus --> Eventually Neutral Stimulus FAILS to evoke Emotional Response
Classical Conditioning:
Repeated pairing of Neutral Stimulus + Emotionally Salient Stimulus --> Eventually Neutral Stimulus evokes Emotional Response
Extinction:
Repeated pairing of Neutral Stimulus + ABSENCE of Emotional Stimulus --> Eventually Neutral Stimulus FAILS to evoke Emotional Response
 prite review
prite review
Neurology
Amnesia
Amnesia preceded by epigastric sensation and fear are associated with electrical abnormality where?
ansewr
Temporal lobe
Memory loss pattern in dissociative amnesia?
answer...
Memory loss occurs for a discrete period of time .
Amnesia characterized by loss of memory of events that occur after onset of etiologic condition or agent
answer
Anterograde
What psychoactive drug produces amnesia?
answer
Alcohol
prite2006
drmahir70- Posts : 25
Points : 59
Reputation : 0
Join date : 2011-10-24
Age : 54
Location : iraq
 prite review
prite review
Visual problem in pituitary tumor compressing optic chiasm>?
Bitemporal Hemianopsia
32 y/o pt 1-month history of worsening headaches, episodic mood swings and occasional hallucinations with visual, tactile and auditory content. CT head reveals tumor where?:
Temporal lobe
Syndrome characterized by fluent speech, preserved comprehension, inability to repeat, w/o associated signs. Location of lesion in the brain?
Supramarginal gyrus or insula
Acute onset of hemiballismus of LUE & LLE. MRI is most likely to show lesion located where?
Subthalamic nucleus
Left sided hemi-neglect is associated with lesion located where?
Right Parietal Lobe
60M right-handed, getting lost, only writes on right half of paper. Where is lesion
Right parietal
Which hormone secreted in functional pituitary adenoma:?
Prolactin
CT & MRI show ventriculomegaly are out of proportion to sulcal atrophy. This is suggestive of what diagnosis?
Normal Pressure Hydrocephalus
5 y/o with 4 month history of morning HA, vomiting, and recent problems with gait, falls, and diplopia?
Medulloblastoma
20 y/o with 1 yr of bitemporal headaches, polydipsia, polyuria, bulimia. For 2 months emotional outburst aggressive and transient confusion neuro exam normal. What will MRI of brain show?
Hypothalamic tumor
Previously pleasant mom becomes profane and irresponsible over 6 months:?
Frontal lobe
Unilateral hearing loss with vertigo, unsteadiness with falls and headaches, mild facial weakness and ipsilateral limb ataxia is most commonly associated with tumors in what locations:?
Cerebellopontine angle
Bitemporal Hemianopsia
32 y/o pt 1-month history of worsening headaches, episodic mood swings and occasional hallucinations with visual, tactile and auditory content. CT head reveals tumor where?:
Temporal lobe
Syndrome characterized by fluent speech, preserved comprehension, inability to repeat, w/o associated signs. Location of lesion in the brain?
Supramarginal gyrus or insula
Acute onset of hemiballismus of LUE & LLE. MRI is most likely to show lesion located where?
Subthalamic nucleus
Left sided hemi-neglect is associated with lesion located where?
Right Parietal Lobe
60M right-handed, getting lost, only writes on right half of paper. Where is lesion
Right parietal
Which hormone secreted in functional pituitary adenoma:?
Prolactin
CT & MRI show ventriculomegaly are out of proportion to sulcal atrophy. This is suggestive of what diagnosis?
Normal Pressure Hydrocephalus
5 y/o with 4 month history of morning HA, vomiting, and recent problems with gait, falls, and diplopia?
Medulloblastoma
20 y/o with 1 yr of bitemporal headaches, polydipsia, polyuria, bulimia. For 2 months emotional outburst aggressive and transient confusion neuro exam normal. What will MRI of brain show?
Hypothalamic tumor
Previously pleasant mom becomes profane and irresponsible over 6 months:?
Frontal lobe
Unilateral hearing loss with vertigo, unsteadiness with falls and headaches, mild facial weakness and ipsilateral limb ataxia is most commonly associated with tumors in what locations:?
Cerebellopontine angle
drmahir70- Posts : 25
Points : 59
Reputation : 0
Join date : 2011-10-24
Age : 54
Location : iraq
 Re: PRITE High Yield Topic Discussion Thread
Re: PRITE High Yield Topic Discussion Thread
Catatonia in prite review
| 52 y/o with h/o unipolar depression is brought to ED with a first episode of catatonia. Patient is on no meds, UDS is neg. Further w/u should initially focus on what factor? | Metabolic disorders |
| Which term describes state of immobility that is constantly maintained? | Cataplexy |
| Ability of catatonic pt to hold same position | Catalepsy |
drmahir70- Posts : 25
Points : 59
Reputation : 0
Join date : 2011-10-24
Age : 54
Location : iraq
 cva in psychiatry prite review
cva in psychiatry prite review
| CVA | |
| Chronic Afib develops aphasia and R hemiparesis at noon. ER exam notes weakness of R extremities and severe dysfluent aphasia, but CT at 1:30 PM has no acute lesion. Most appropriate treatment: | TPA |
| Young adult gained 70 lbs in last year c/o daily severe headaches sometimes assoc with graying out of vision. Papilledema present. CT and MRI brain no abnormalities but ventricles smaller than usual. Goal of treatment in this case: | Prevent blindness |
| Patient with hypertension develops vertigo, nausea, vomiting, hiccups, left sided face numbness, nystagmus, hoarseness, ataxia of the limbs, staggering gait, and is falling to the left. Dx? | Lateral medullary stroke |
| Rapid onset of right facial weakness, left limb weakness, diplopia | Brain Stem Infarction |
| Transient symptom associated with carotid stenosis: *** | Monocular blindness |
| 62 y/o M w DM is not making sense, saying “thar szing is phrumper zu stalking”. Normal intonation but no one in the family can understand it. He verbally responds to questions with similar utterances but fails to successfully execute any instruction. **** | Wernicke’s aphasia |
| 58 y/o M h/o HTN, cig smoking and sudden inability to speak. Face drooping on R and dragging R leg. In ER examined within 40 mins of onset: Aphasic, unable to understand or repeat verbal commands. Unintelligable sounds for speech. Alert but appeared frustrated. R hemiplegia with arm and face weaker than leg. CT head showed no hemorrhage. Pathology type and area: | Thromboembolic stroke L MCA (middle cerebral artery) |
| Abulia refers to impairment in ability to: | Spontaneously move and speak |
| Sudden-onset left hemiparesis with deviation of eyes to the right | Right putaminal hemorrhage |
| Sudden onset vertigo/nausea, hoarseness/dysphagia, right sided face numbness, diminished gag reflex on right, decreased pinprick and temp sensation on left | Right medullary infarction |
| 65 y/o diabetic presents to ED c/o acute L sided weakness, deviation of gaze to R, L hemiplegia and hemisensory deficit, and L homonymous hemianopsia. 12 hrs later, pt is unconscious, L pupil enlarged and unreactive. CT will show what? | R MCA infarct w/ edema and uncal herniation |
| Pt with acute onset vertigo, what will suggest R lateral medullary infarct? | R facial loss of touch + temp sensation |
| 46 y/o M w/ double vision + pain R eye. Exam: ptosis R eyelid, inability to elevate or adduct R eye + R pupillary dilation. This is caused by: | Post. Communicating artery aneurysm |
| Aphasia w/ effortful fragmented, dysfluent, telegraphic speech, is seen in a lesion where? | Post frontal lobe |
| 39 year old with h/o of multiple miscarriages develops an acute left sided hemiparesis. Work up revels elevated anticardiolipin titers and no other risk factors for stroke. Appropriate intervention at this point is? | Plasmapheresis |
| Abnormal elevated metabolic findings associated with increased risk of stroke in patients under 50 | Plasma homocysteine |
| 73 y/o found on floor, unaware of L UE/LE. Flaccid L arm, but denies anything wrong and when asked to raise L arm raises R. When asked which arm is her L, she replies “yours.” Dx? | Parietal lobe CVA |
| CT scan with occipital and intraventricular hyperintensities | Parenchymal hemorrhage |
| Which med has secondary prevention against embolic stroke in patients with Afib? | Oral warfarin |
| As opposed to strokes caused by arterial embolism or thrombosis, those caused by cerebral vein or venous sinus thrombosis are | More often associated with seizures at onset |
| Atrophy of right temporal lobe on cross section associated with occlusion of: | Middle cerebral artery |
| Loss of ability to execute previously learned motor activities (which is not the result of demonstrable weakness, ataxia or sensory loss) is associated with lesions of? | Left parietal cortex |
| 58 y/o s/p CABG – anomia for fingers and body parts, errors involving right and left, inability to write thoughts/take notes/make calculations. Fluent speech and excellent comprehension | Left medial temporal stroke |
| Visual disturbances associated with occlusion of the right posterior cerebral artery? | Left homonymous hemianopsia |
| 65 y/o with HTN collapsed. In ED is stuporous, R hemiparesis + hemisensory deficit, eyes deviate to L. CT would show intraparenchymal hemorrhage in: | Left basal ganglia |
| Higher frequency & greater severity of depression associated w/ cortical & subcortical strokes | Left anterior frontal |
| Pt with hypertension develops painless vision loss on the left eye. PE revels blindness in the left eye and afferent papillary defect on the left. MRI shows several T2 hyperintensities in the white matter periventricularly. No corpus callosum lesions. No enhancement with gadolinium. Dx? | Ischemic optic neuropathy |
| 63 y/o with new onset aphasia and R hemiparesis, 2 days ago had milder/similar symptoms that resolved in 30 minutes, yesterday had similar episode x45 minutes. Current sx started 1.5 hrs ago. CT shows no stroke or hemorrhage. Tx? | Intravenous thrombolytic agents |
| Lower facial weakness w/ relative sparing of forehead can be stroke in | Internal capsule |
| Prosopagnosia is: | Inability to recognize faces |
| 57 y/o diabetic w/ HTN c/o several episodes of visual loss “curtain falling” over his L eye, transient speech and language disturbance, and mild R hemiparesis that lasted 2 hrs. Suggests presence of what? | Extracranial L internal carotid stenosis |
| Head injury with LOC followed by lucid interval for a few hours then rapidly progressing coma. What hemorrhage? | Epidural |
| 5 days after CABG a 47 yr M is disoriented in time and place. He identifies his right and left but not that of the examiners. Can draw square and circle but not a clock. This is: | Dyspraxia |
| Pt in ED with sudden HA and collapsing, some lethargy. Exam shows rigid neck, no papilledema, no focal CN or motor signs. The initial test should be? | CT Head |
| Post stroke depression in an 80 y/o pt who is R handed is associated with cognitive impairments that | Correlate with left hemispheric involvement |
| Fluent speech with preserved comprehension but inability to repeat statements is consistent with what type of aphasia? | Conduction |
| Normal Romberg w eyes open but loses balance with eyes closed. Where is abnormality? | Cerebellar vermis |
| 65 y/o with h/o HTN, Meniere’s with sudden vertigo, N/V, worse with head movement, R beating nystagmus on lateral gaze, finger to nose testing is ataxic, poor balance and dysarthria. Dx? | Cerebellar infarct |
| 66 y/o M in ED w/ sudden occipital HA, dizziness, vertigo, N/V, unable to stand, mild lethargy, slurred speech. Exam shows small reactive pupils, gaze deviated to the R, nystagmus, w/ occasional ocular bobbing, R facial weakness, decreased R corneal reflex, truncal ataxia, b/l hyperreflexia, b/l Babinski. Dx? | Cerebellar hemorrhage |
| Motor speech paradigm activation task on fMRI – hyperactivity in right temporal lobe. Damage is where? | Calcarine fissure |
| Inability to recognize objects by touch: | Astereognosis |
| In managing acute ischemic stroke, administer this within 48 hrs of onset of stroke for beneficial effect in reducing risk of recurrent stroke, disability and death: | Aspirin |
| 70 y/o w/ attacks of “whirling sensations” w/n/v, diplopia, dysarthria, tingling of lips. Occurs several times daily for 1 minute, severe that pt collapses and is immobilized when symptoms start. No residual s/s, no tinnitus, hearing impairment, ALOC or association with any particular activity. Dx? | Vertebrobasilar insufficiency |
| Component of type A behavior most reliable risk factor for CAD | Hostility |
| 70 y/o F sudden onset paralysis R foot and leg. R arm and hand lightly affected. No aphasia or visual field deficit. Over weeks found with loss bladder control, abulia and lack of spontaneity. Which vascular area: | Anterior cerebral artery (left) |
| Complications of a cerebellar hemorrhage? | Acute hydrocephalus |
drmahir70- Posts : 25
Points : 59
Reputation : 0
Join date : 2011-10-24
Age : 54
Location : iraq
 dementia prite review
dementia prite review
| Delirium | |
| Multifocal myoclonus in a comatose patient indicates: | Metabolic Encephalopathy |
| 50M male w/ progressive dementia, ataxia, dysarthria, EEG w/ sharp waves | Subacute Spongiform Encephalopathy |
| 79 y/o with decreasing mental state over 3 weeks has an exaggerated startle response with violent myoclonus that is elicited by turning on the room lights, speaking loudly, or touching the patient. Myoclonic jerks occur spontaneously. Dx? | Spongiform Encephalopathy |
| Two days after bowel surgery, 53 y/o is delirious. Correctly draws a square when asked, but then continues to draw squares when asked to draw other shapes. MSE would reveal: | Perseveration |
| 75 y/o F is 8 days s/p total hip replacement and has delirium. Her diazepam and doxepin were discontinued just prior to surgery. She is getting meperidine for pain, diphenhydramine for sleep and a renewed prescription for doxepin. Her confusion is likely due to: medication toxicity, diazepam WDRL, electrolyte imbalance, atypical depression, UTI. | Medication toxicity, diazepam withdrawal, electrolyte imbalance, atypical depression, or UTI. |
| Best recommendation for pt with delirium? Minimize contact with family members or limit sleep meds to diphenhydramine, or maximize staff continuity assigned to pt? | Maximize staff continuity assigned to pt |
| Delirium in HIV patients treated with what parental agent? | Low dose of a high-potency antipsychotic |
| Mild confusion, lethargy, thirst, polydipsia | Hyponatremia |
| Cancer patient on chemo is disoriented and agitated. Afebrile VSS. Neg neuro exam. Poor attention, cog impairment. Held for observation. CT neg, EEG diffuse slowing. Treat with: | Haldol |
| A 70 y/o +HIV heroin abuser is treated with Lopinavir and Ritonavir and fluoxetine for MDD. Hep C was dx and treated 2 months ago. Since then pt is more irritable, insomnia, and diarrhea. Why? | Drug-drug interaction |
| A consult is requested for an inpatient on a medical ward who is agitated and hallucinating. Pt appears to be flushed and hot with dry skin, mydriasis, a rapid pulse and diminished bowel sounds. What is your first recommendation? | Discontinue anticholinergic drugs |
| 52 y/o w/ depression and HTN, severe headaches, “not himself” x 10 days. Poor eye contact, inattentive, picking at clothes, muttering, nodding off | Delirium |
| Suggests delirium rather than dementia | Clouding of consciousness |
| Dementia | |
| 65 y/o M 6 months confusion episodes, disorientation, visual hallucinations of children playing in his room. Hallucinated images are fully formed, colorful, vivid and pt has little insight into their nature. No AH. Wife says he is normal between episodes. Exam: Normal language, memory, mod diff with trails test, mild diff with serial subtractions, mild symmetric rigidity and bradykinesia. Brain MRI unremarkable. CSF, routine labs and UDS normal. Diagnosis: | Lewy body dementia |
| Dementing illness with limb and axial rigidity tremor, fluctuations in cognitive function, confusion states, hallucinosis and other symptoms of psychosis. Dx? | Diffuse lewy body disease |
| 70 y/o woman has dementia, abnormal proprioception, and dysesthesia. Lab studies reveal macrocytic anemia most likely caused by a deficiency of | Vitamin B12 |
| 74F PI, suspicious, poor ADL’s | Pick’s disease |
| Safest heterocyclic antidepressant for a 78 y/o with depression, agitation and dementia is: | Nortriptyline |
| What cognitive enhancers is an NMDA receptor antagonist? | Memantine |
| Neuronal damage from excitotoxicity secondary to glutamate sensitivity. Treat with: | Memantine |
| 75 y/o with mild intermittent forgetfulness, hallucinations, delusions, confusion. Frequent falls and dizziness when getting out of bed. BP laying down 135/90, standing 100/55. BL limb and axial rigidity without tremor. Dx? | Lewy Body disease |
| Detection of 2 Apolien e4 alleles is useful in dx dementia b/c | Increases probability of dx of Alzheimers |
| Neurofibrillary tangles in Alzheimer’s are composed of: | Hyperphosphorylated tau proteins |
| 80 y/o Alzheimer’s with increasingly combative behavior. Family wants to keep at home. Give what med? | Haldol |
| Dementia characterized by personality change, attention deficits, impulsivity, affect lability, indifference, perseveration, loss of executive function. Assoc with dysfunction in what area of the brain? | Frontal lobe |
| Alzheimer’s disease risk – Apolipoprotein E phenotype | ɛ4ɛ4 |
| Binswanger disease has pseudobulbar state, gait disorder, AND: | Dementia |
| An 80yo pt with Alzheimer’s is brought in for increasingly combative behavior. Daughter would like to keep the pt at home if possible. What interventions would be most helpful in this situation? | Assessing for caregiver burnout |
| Which meds have best results for treating agitation in dementia? | Anti-psychotics |
| Clock drawing test is quickly administered and sensitive screen for which d/o? | Alzheimer’s |
| Amyloid precursor protein in | Alzheimer’s Disease |
| Most common cause of dementia: | Alzheimer’s disease |
| Individuals over 40yo with Down’s syndrome frequently develops: | Alzheimer’s |
| What baseline labs should be taken before starting tacrine? | ALT and AST (baseline and f/u) |
| Known risk factors for dementia: | Age, family hx, female, Down Syndrome |
| Neuronal enzyme that is the target of drugs to treat Alzheimer’s i.e. galantamine and rivastigmine | Acetyl cholinesterase |
drmahir70- Posts : 25
Points : 59
Reputation : 0
Join date : 2011-10-24
Age : 54
Location : iraq
 seizure prite review
seizure prite review
| Seizures | |
| 19 yr old woman has bouts of motor agitation, often followed by intense, seemingly meaningless writing; also mood lability, tactile & olfactory hallucinations. During the interview, patient abruptly stops paying attention and begins rapidly pacing around the room. What should be the next step? | Wait 15 mins, then obtain prolactin level |
| Which procedure confirms the diagnosis of non-epileptic seizures? Video telemetry or EEG between episodes? | Video telemetry (CL: Should be more accurately called EEG Video telemetry) |
| Antiepileptic for juvenile myoclonic epilepsy | Valproic Acid |
| Complex partial seizures are differentiated from simple partial seizures by: | Simple seizures have no loss of consciousness but have altered responsiveness to outside stimuli. |
| Convulsive episode with leftward eye deviation, tonic contracture of left side. Postictally, eyes deviate to right w/ hemiparesis of left side | Seizure focus right frontal region |
| 28 female w/ HA, hyperventilates, asynchronous tonic-clonic sz, no LOC during Sz | Psychogenic Seizure |
| In young pt w/ epilepsy, tx depression w/ | Prozac |
| Lack of prolactin elevation after szs suggests what kind of szs: | Non-epileptic |
| 32 y/o with partial complex seizures refractory to treatment, picture of MRI shown. (picture) | Mesial temporal sclerosis |
| Drug-addicted healthcare professional experiences seizure that is not a withdrawal phenomenon. Cause? | Meperidine |
| What is the diagnostic value of transient paresis or aphasia after a seizure? | Localizes the focus of seizure |
| Complex partial epilepsy aura has what symptom? | Lip smacking |
| Head & eyes deviate to right and right arm extends immediately before a generalized tonic-clonic seizure | Left cerebral hemisphere |
| Gustatory special sensory seizures (auras) localize where? | Insular cortex |
| First sz with focal onset and second generalization in a 58 y/o patient is most likely the consequence of what? | Glioblastoma multiforme |
| 10 y/o child freq episodes brief lapses of consciousness without premonitory sxs. Lasts 2-10 seconds, followed by immediate and full resumption of consciousness without awareness of what has happened. These ictal episodes most likely caused by what kind szs: | Absence |
drmahir70- Posts : 25
Points : 59
Reputation : 0
Join date : 2011-10-24
Age : 54
Location : iraq
 Re: PRITE High Yield Topic Discussion Thread
Re: PRITE High Yield Topic Discussion Thread
Obsessive-compulsive disorders-
Notes from lecture conference:
https://psychiatry.forumotion.com/t226-obsessive-compulsive-disorder-notes-from-lecture-conference#394
Notes from lecture conference:
https://psychiatry.forumotion.com/t226-obsessive-compulsive-disorder-notes-from-lecture-conference#394
 Re: PRITE High Yield Topic Discussion Thread
Re: PRITE High Yield Topic Discussion Thread
ROLE OF ZIPRASIDONE IN COMBINATION THERAPY FOR BIPOLAR MAINTENANCE


 Psychiatry Boards and PRITE Question Bank!
Psychiatry Boards and PRITE Question Bank!
I have been using BoardVitals Psychiatry Question Bank to prepare for the PRITE and it is really great so I wanted to share the link. They use the FRED interface (same as we used for USMLE exams) and it has tons of options to make your own tests by subjects within psychiatry, keywords, incorrectly answered etc. It also gives you feedback by subject so you can track how you are doing and focus on your weak subjects. www.BoardVitals.com
sp2010- Posts : 1
Points : 1
Reputation : 0
Join date : 2011-11-07
 Re: PRITE High Yield Topic Discussion Thread
Re: PRITE High Yield Topic Discussion Thread
Basics of Nor-Epinephrine, Dopamine & Seretonin Neurons.
http://bit.ly/uoDyEz
http://bit.ly/uoDyEz
 Re: PRITE High Yield Topic Discussion Thread
Re: PRITE High Yield Topic Discussion Thread
Hyperprolactinaemia With Antipsychotics
http://www.medsafe.govt.nz/profs/puarticles/hyperpro.htm#Atypical
http://www.medsafe.govt.nz/profs/puarticles/hyperpro.htm#Atypical
 Re: PRITE High Yield Topic Discussion Thread
Re: PRITE High Yield Topic Discussion Thread
United Kingdom Parkinsons Disease Society Brain Bank clinical diagnostic criteria
Step 1. Diagnosis of a parkinsonian syndrome
- Bradykinesia and at least one of the following:
- Muscular rigidity
- Rest tremor (4-6 Hz)
- Postural instability unrelated to primary visual, cerebellar,
- vestibular or proprioceptive dysfunction
Step 2. Exclusion criteria
- History of:
* Cerebrovascular disease with stepwise progression
* Repeated head injury
* Antipsychotic or dopamine-depleting drugs
* Definite encephalitis and/or oculogyric crises on no drug treatment
- More than one affected relative
- Sustained remission
- Negative response to large doses of levodopa (if malabsorption excluded)
- Strictly unilateral features after three years
- Other neurological features: supranuclear gaze palsy, cerebellar signs, early severe autonomic involvement, Babinski sign, early severe dementia with disturbances of language, memory or praxis
- Exposure to known neurotoxin
Step 3. Supportive criteria **Imp**
- Unilateral onset
- Excellent response to levodopa
- Rest tremor present
- Progressive disorder
- Persistent asymmetry, affecting side of onset most
- Severe levodopa-induced chorea
- Levodopa response for five years plus
- Clinical course of 10 years plus
Source: Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. JNeurol Neurosurg Psychiatry 1992; 55: 181-184.
Step 1. Diagnosis of a parkinsonian syndrome
- Bradykinesia and at least one of the following:
- Muscular rigidity
- Rest tremor (4-6 Hz)
- Postural instability unrelated to primary visual, cerebellar,
- vestibular or proprioceptive dysfunction
Step 2. Exclusion criteria
- History of:
* Cerebrovascular disease with stepwise progression
* Repeated head injury
* Antipsychotic or dopamine-depleting drugs
* Definite encephalitis and/or oculogyric crises on no drug treatment
- More than one affected relative
- Sustained remission
- Negative response to large doses of levodopa (if malabsorption excluded)
- Strictly unilateral features after three years
- Other neurological features: supranuclear gaze palsy, cerebellar signs, early severe autonomic involvement, Babinski sign, early severe dementia with disturbances of language, memory or praxis
- Exposure to known neurotoxin
Step 3. Supportive criteria **Imp**
- Unilateral onset
- Excellent response to levodopa
- Rest tremor present
- Progressive disorder
- Persistent asymmetry, affecting side of onset most
- Severe levodopa-induced chorea
- Levodopa response for five years plus
- Clinical course of 10 years plus
Source: Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. JNeurol Neurosurg Psychiatry 1992; 55: 181-184.
Page 3 of 4 •  1, 2, 3, 4
1, 2, 3, 4 
 Similar topics
Similar topics» PRITE Discussion Thread- 2013
» Supportive Psychotherapy- High Yield Facts
» Personality Disorders (10 High Yield Facts)
» prite exam
» PRITE Oriented Topics
» Supportive Psychotherapy- High Yield Facts
» Personality Disorders (10 High Yield Facts)
» prite exam
» PRITE Oriented Topics
FORUM FOR PSYCHIATRY RESIDENTS :: Psychiatry :: Psychiatry-Neurology-Psychology discussion :: Psychiatry In Depth
Page 3 of 4
Permissions in this forum:
You cannot reply to topics in this forum






» L-Methylfolate: Who Will benefit
» Vitamins & Supplements in Clinical Practice.
» Imaging Biomarkers for Outcomes in Mild TBI
» Q.5 Clozapine Neutopenia
» Treating Disorders!
» Cortical Abnormalities in Adults & Adolescents with MDD
» Efficacy of Antipsychotics in Pediatric Acute Mania
» Obsessive Compulsive Disorder in Adults: Which Treatment is Better?