
Search
Statistics
We have 222 registered usersThe newest registered user is raheelmemon
Our users have posted a total of 1140 messages in 613 subjects
If you are seeing this, you have attempted to link to the UpToDate widget but are experiencing a problem. Please visit UpToDate for more information.
Schizophrenia- In Depth Explanation & Discussion
FORUM FOR PSYCHIATRY RESIDENTS :: Psychiatry :: Psychiatry-Neurology-Psychology discussion :: Psychiatry In Depth
Page 1 of 1
 Schizophrenia- In Depth Explanation & Discussion
Schizophrenia- In Depth Explanation & Discussion
Schizophrenia- In Depth Explanation & Discussion
Harvinder Singh, M.D


Harvinder Singh, M.D


Hi Friends,
This thread is dedicated to discussion of topics specific to Schizophrenia. Everyone is encouraged to participate.

Check the "Topic Index" below for updated posts daily.
Topic Index:
Page-1:
1. DSM-IV-TR Diagnostic Criteria for Schizophrenia.
2. Clinical Features of Schizophrenia (with examples).
3. Subtypes of Schizophrenia.
4. Neuroanatomy Changes: First Episode vs Chronic Schizophrenia.
5. Phencyclidine Model of Schizophrenia.
6. Differential Diagnosis.
7. Role of Dopamine, Serotonin & NE Pathways in Schizophrenia.
8. Videos: Patient's View on Schizophrenia.
9. Early Detection of Schizophrenia: Current Evidence and Future Perspectives
10. Effectiveness of Clozapine Versus Olanzapine, Quetiapine, and Risperidone in Patients With Chronic Schizophrenia Who Did Not Respond to Prior Atypical Antipsychotic Treatment.
11. Long-term Antipsychotic Treatment and Brain Volumes in First-Episode Schizophrenia.
12. Relapse prevention in schizophrenia: second-generation antipsychotics versus first-generation antipsychotics
13. Childhood Onset Schizophrenia- HY Facts
14. Catatonia
Page-2:
15. Polypharmacy With Antipsychotics, Antidepressants, or Benzodiazepines and Mortality in Schizophrenia
16. Haldol Decanoate- Dosing Strategies
17. Abnormal Involuntary Movement Scale (AIMS)
18. Treatment of Schizophrenia With Long-Acting Fluphenazine, Haloperidol, or Risperidone
19. Coming Soon ...
20. Coming Soon ...
Last edited by Admin on Sun Feb 17, 2013 4:48 pm; edited 26 times in total
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
1. DSM-IV-TR Diagnostic Criteria for Schizophrenia
A. Characteristic symptoms: Two (or more) of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated):
- Delusions
- Hallucinations
- Disorganized speech (e.g., frequent derailment or incoherence)
- Grossly disorganized or catatonic behavior
- Negative symptoms, i.e., affective flattening, alogia, or avolition
Note: Only one Criterion A symptom is required if:
- delusions are bizarre or
- hallucinations consist of a voice keeping up a running commentary on the person's behavior or thoughts, or
- two or more voices conversing with each other.
B. Social/occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care are markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, failure to achieve expected level of interpersonal, academic, or occupational achievement).
C. Duration: Continuous signs of the disturbance persist for at least 6 months.
This 6-month period must include at least 1 month of symptoms (or less if successfully treated) that meet Criterion A (i.e., active-phase symptoms) and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or two or more symptoms listed in Criterion A present in an attenuated form (e.g., odd beliefs, unusual perceptual experiences).
D. Schizoaffective and mood disorder exclusion: Schizoaffective disorder and mood disorder with psychotic features have been ruled out because either
(1) no major depressive, manic, or mixed episodes have occurred concurrently with the active-phase symptoms; or
(2) if mood episodes have occurred during active-phase symptoms, their total duration has been brief relative to the duration of the active and residual periods.
E. Substance/general medical condition exclusion: The disturbance is not due to the direct physiological effects of a substance (e.g., a drug of abuse, a medication) or a general medical condition.
F. Relationship to a pervasive developmental disorder: If there is a history of autistic disorder or another pervasive developmental disorder, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations are also present for at least a month (or less if successfully treated).
A. Characteristic symptoms: Two (or more) of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated):
- Delusions
- Hallucinations
- Disorganized speech (e.g., frequent derailment or incoherence)
- Grossly disorganized or catatonic behavior
- Negative symptoms, i.e., affective flattening, alogia, or avolition
Note: Only one Criterion A symptom is required if:
- delusions are bizarre or
- hallucinations consist of a voice keeping up a running commentary on the person's behavior or thoughts, or
- two or more voices conversing with each other.
B. Social/occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care are markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, failure to achieve expected level of interpersonal, academic, or occupational achievement).
C. Duration: Continuous signs of the disturbance persist for at least 6 months.
This 6-month period must include at least 1 month of symptoms (or less if successfully treated) that meet Criterion A (i.e., active-phase symptoms) and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or two or more symptoms listed in Criterion A present in an attenuated form (e.g., odd beliefs, unusual perceptual experiences).
D. Schizoaffective and mood disorder exclusion: Schizoaffective disorder and mood disorder with psychotic features have been ruled out because either
(1) no major depressive, manic, or mixed episodes have occurred concurrently with the active-phase symptoms; or
(2) if mood episodes have occurred during active-phase symptoms, their total duration has been brief relative to the duration of the active and residual periods.
E. Substance/general medical condition exclusion: The disturbance is not due to the direct physiological effects of a substance (e.g., a drug of abuse, a medication) or a general medical condition.
F. Relationship to a pervasive developmental disorder: If there is a history of autistic disorder or another pervasive developmental disorder, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations are also present for at least a month (or less if successfully treated).
Last edited by Admin on Sat May 19, 2012 8:54 pm; edited 1 time in total
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
2. Clinical Features:
* Delusions:
Delusions of persecution:
Ex- There is a conspiracy against the patient; The patient is followed by cars; headlights blink on and off to indicate that capture is imminent; The food is poisoned.
One patient who believed that persecutors sent electrical charges down through the ceiling at night papered the entire ceiling with aluminum foil and for a time felt protected.
Grandiose delusions:
often in conjugation with delusions of persecution.
Ex:- the angel of the Lord has visited them. They embark for Washington; the President wishes their advice. Commonly most patients do not act on their delusions; Exceptions do occur- One patient announced a plan for world happiness in a full-page newspaper ad; another sent a letter of advice to the Secretary of State.
Delusions of reference:
Here patients believe that otherwise chance occurrences or random encounters have special meaning for them.
Ex: The street lights blink on; it is a sign for the persecutors to close in for the final attack. The television newscaster speaks in code; the songs on the radio hold special meaning for the patient.
Also inquire about thought broadcasting, thought withdrawal, and thought insertion.
Patients who experience this symptom of thought withdrawal may concurrently, if they happen to be speaking their thoughts, display the sign known as “thought blocking.”
Delusion of doubles, also known as the “Capgras phenomenon,” or the delusion of impostors:
Here the patient believes that someone, or something, has occupied the body of another.
* Disorganized speech
- Focus on form of speech rather than content of the patient’s speech.
- Loosening of associations (less frequently it is referred to as incoherence or “derailment.”):
The patient’s speech becomes illogical; family member may say that the patient “doesn’t make sense.” At its extreme, it may present as a “word salad.”
Ex: patient was asked to report the previous day’s activities; the patient replied, in part, “The sun bestrides the mouse doctor. In the morning, if you wish. Twenty-five dollars is a lot of money! Large faces and eyes. Terrible smells. Rat in the socket. Can there be darkness? Oh, if you only knew!” thoughts here are no longer “goal-directed”;
Interestingly, also, these patients seem little concerned about their incoherence. They seem oblivious to it and make little if any effort to clarify what they say.
- Neologisms:
These are words that occur in the normal course of the patient’s speech, but that convey no more meaning to the listener
To the patient, however, they have as much meaning and status as any other word
Ex: One patient was offered a cup of coffee, the reply was, “Yes, doctor, thank you. With bufkuf.” When asked the meaning of “bufkuf,” the patient replied “Oh, you know,” and made no further effort to define or explain it.
* Catatonic symptoms
- Negativism:
Characterized by a mulish, automatic, almost instinctual opposition to any course of action suggested, demanded, or merely expected.
In some cases this negativism is passive. Ex: if food is placed in front of patients, they do not
eat; if their clothes are set out for them, they do not dress; if a question is asked, they do not answer
In more extreme cases the negativism becomes active, and patients may do the exact
opposite of what is expected. Ex: if shown to their room, they may enter another; if asked to open their mouths, they may clamp shut; if asked to walk from a burning room, they may walk back in.
In some patients one may see the exact opposite of negativism “automatic obedience.” Here, patients do whatever they are told to do, regardless of what it is. In the nineteenth century, one way to test for this symptom was to tell a patient that you wished him to stick the tongue out so that it might be pierced with a needle. Patients would protrude their tongues and not flinch when pierced by the needle.
- Catalepsy (waxy flexibility):
State of continual and most unusual muscular tension.
Ex: If one attempts to bend the patient’s arm, it is as if one were bending a length of thick metal wire, like soldering wire. The remarkable aspect here is that, as in bending the wire, the patient retains whatever position the limb, or for that matter, the body, is placed in.
This symptom, rarely seen in modern times, was common before the advent of antipsychotic medicines in the middle of the twentieth century.
- Stereotypies:
bizarre, perseverated behaviors.
Ex: patient may march back and forth along the same line for hours; another may repeatedly dress and undress. Other persons may be approached again and again, each time being asked the same question. The same piece of paper may be folded and unfolded until it disintegrates. Most patients can offer no reason for their senseless activity. When asked, a patient replied, “it must be so.”
- Echolalia and echopraxia:
patient’s behavior mirrors that of the other person, and, importantly, when this happens automatically, and in the absence of any request.
If asked a question the echolalic patient will simply repeat it, sometimes over and over again.
The echopraxic patient may clumsily mirror the gestures and posture of the interviewer and, as in echolalia, may continue to do this long after the other person has left, as if uncontrollably compelled to maintain the same activity.
* Bizarre behavior:
- Mannerisms:
bizarre or odd caricatures of gestures, speech, or behavior.
Ex: In manneristic gesturing- patients may offer their hands to shake with the fingers splayed out, or the fingers may writhe in a peculiar, contorted way.
In manneristic speech- cadence, modulation, or volume are erratic and dysmodulated. One patient may speak in a singsong voice, another in a telegraphic style, and yet another with pompous accenting of random syllables.
In manneristic behavior- rather than walking, some patients may march in bizarre, stiff-legged fashion.
- Bizarre affect:
represent a distortion of the normal connection between felt emotion and affective expression.
facial expression appears theatrical, wooden, or under a peculiar constraint.
Patients may report feeling joy, yet the rapturous facial expression may appear brittle and tenuous.
Conversely patients may report grief, and indeed tears may be present, yet the emotion lacks depth, as if patients were merely wearing a mask of grief that might disappear at any moment.
Another, very important form of bizarre affect is unprovoked and mirthless laughter. For no apparent reason patients may break into bizarre and unrestrainable laughter. Though appearing neither happy nor amused, the laughter continues.
- Inappropriate affect may also be seen:
Here the connection between the patient’s ideas and affect seems completely severed.
A young patient, grief stricken at a parent’s funeral, was seen to snicker; another patient, relating the infernal tortures suffered just the night before, smiled beatifically.
- Deterioration of behavior:
Patients become untidy and may neglect to bathe or wash their clothes; the fingernails may become very long. Dress and grooming may become bizarre. Several layers of clothing are often worn, even during the summer. Bits of string or cloth may festoon the patient’s hair or garments; makeup may be smeared on.
Not uncommonly, paranoid patients shave their heads, and this often reliably predicts an oncoming
exacerbation of illness, and also some form of selfmutilation.
Patients may pluck out their eyelashes or cut deep gouges in their legs.
Some seem to be almost completely analgesic: an eye may be plucked out; pieces of flesh may be
bitten off; in extreme cases, self-evisceration may occur, “just to see” what the intestines look like.
* Negative symptoms:
- Flattening of affect (when less severe- “blunting” of affect)
Characterized by a lifeless and wooden facial expression accompanied by an absence or diminution of all feelings.
This is quite different from a depressed appearance. In depression patients appear drained or weighted down; there is a definite sense of something there.
In flattening, however, patients seem to have nothing to express; they are simply devoid of emotion. They appear unmoved, wooden, and almost at times as if they were machines.
Poverty of speech:
patients, though perhaps talking a normal amount, seem to “say” very little.
There is a dearth of meaningful content to what they say and speech is often composed of stock phrases and repetitions.
Poverty of thought:
characterized by a far-reaching impoverishment of the entire thinking of the patient.
patient may complain of having “no thoughts,” that “the head is empty,” that there are no “stirrings.” Of its own accord nothing “comes to mind.”
If pressed by a question the patient may offer a sparse reply, then fail to say anything else.
Avolition (referred to by Kraepelin as “annihilation of the will”):
It is said to be present when patients have lost the capacity to embark on almost any goal-directed activity.
Ex: Bills are not paid; the house is not cleaned; infants are neither changed nor fed. This is not because patients feel inhibited, lack interest, or suffer from fatigue, but rather because the ability to will an action has become deficient.
Ambivalence:
may render patients incapable of almost any volitional activity.
Here, patients experience two opposed courses of action at the same time, and for lack of ability to decide between them, do nothing.
Ex: One patient stood at the washstand for hours unable to decide whether to shave or to use the toothbrush.
This “paralysis of will,” however, may at times be easily removed if another person gives directions. In
this case an aide simply told the patient to brush his teeth and then put the toothbrush in the patient’s hand. Immediately and with peculiar alacrity the patient then set to brushing his teeth.
Imp- This kind of ambivalence found in schizophrenia is to be distinguished from the indecisiveness seen at times in depression and the “normal” ambivalence that anyone may experience.
The depressed patient’s inability to embark on decision-making stems more from a lack of energy and
initiative; unlike the patient with schizophrenia, the depressed patient generally is not able to act when others make the decision.
In normal circumstances competing desires may leave the patient unable to decide. With time, however, a normal person makes a decision because the capacity to do so is not lost. In schizophrenia, however, it is this very capacity that is no longer present.
“Double bookkeeping” :
refers to the patient’s ability to, as it were, live in two worlds at the same time.
On the one hand is the world of voices, visions, and delusions, and on the other hand, and quite coincident with this psychotic world, is the world as perceived by others. To the patient both worlds seem quite real.
Ex: a patient may hear a voice as clearly as the voice of the physician and believe it just as real, yet at the same time acknowledge that the physician does not hear it.
Or the grandiose patient who fully believed that a coronation was imminent may yet continue to work at a janitor’s job and go on doing so, living in two worlds, and feeling little if any conflict between them.
A variant of double bookkeeping, known as “double orientation,” or “delusional disorientation,” may at times mislead the interviewer into thinking that the patient is disoriented.
Ex: grandiose patient believed that he was John F. Kennedy, and when asked what year it was replied 1962. Later on, however, when filling out a form, he put down the correct year.
* Delusions:
Delusions of persecution:
Ex- There is a conspiracy against the patient; The patient is followed by cars; headlights blink on and off to indicate that capture is imminent; The food is poisoned.
One patient who believed that persecutors sent electrical charges down through the ceiling at night papered the entire ceiling with aluminum foil and for a time felt protected.
Grandiose delusions:
often in conjugation with delusions of persecution.
Ex:- the angel of the Lord has visited them. They embark for Washington; the President wishes their advice. Commonly most patients do not act on their delusions; Exceptions do occur- One patient announced a plan for world happiness in a full-page newspaper ad; another sent a letter of advice to the Secretary of State.
Delusions of reference:
Here patients believe that otherwise chance occurrences or random encounters have special meaning for them.
Ex: The street lights blink on; it is a sign for the persecutors to close in for the final attack. The television newscaster speaks in code; the songs on the radio hold special meaning for the patient.
Also inquire about thought broadcasting, thought withdrawal, and thought insertion.
Patients who experience this symptom of thought withdrawal may concurrently, if they happen to be speaking their thoughts, display the sign known as “thought blocking.”
Delusion of doubles, also known as the “Capgras phenomenon,” or the delusion of impostors:
Here the patient believes that someone, or something, has occupied the body of another.
* Disorganized speech
- Focus on form of speech rather than content of the patient’s speech.
- Loosening of associations (less frequently it is referred to as incoherence or “derailment.”):
The patient’s speech becomes illogical; family member may say that the patient “doesn’t make sense.” At its extreme, it may present as a “word salad.”
Ex: patient was asked to report the previous day’s activities; the patient replied, in part, “The sun bestrides the mouse doctor. In the morning, if you wish. Twenty-five dollars is a lot of money! Large faces and eyes. Terrible smells. Rat in the socket. Can there be darkness? Oh, if you only knew!” thoughts here are no longer “goal-directed”;
Interestingly, also, these patients seem little concerned about their incoherence. They seem oblivious to it and make little if any effort to clarify what they say.
- Neologisms:
These are words that occur in the normal course of the patient’s speech, but that convey no more meaning to the listener
To the patient, however, they have as much meaning and status as any other word
Ex: One patient was offered a cup of coffee, the reply was, “Yes, doctor, thank you. With bufkuf.” When asked the meaning of “bufkuf,” the patient replied “Oh, you know,” and made no further effort to define or explain it.
* Catatonic symptoms
- Negativism:
Characterized by a mulish, automatic, almost instinctual opposition to any course of action suggested, demanded, or merely expected.
In some cases this negativism is passive. Ex: if food is placed in front of patients, they do not
eat; if their clothes are set out for them, they do not dress; if a question is asked, they do not answer
In more extreme cases the negativism becomes active, and patients may do the exact
opposite of what is expected. Ex: if shown to their room, they may enter another; if asked to open their mouths, they may clamp shut; if asked to walk from a burning room, they may walk back in.
In some patients one may see the exact opposite of negativism “automatic obedience.” Here, patients do whatever they are told to do, regardless of what it is. In the nineteenth century, one way to test for this symptom was to tell a patient that you wished him to stick the tongue out so that it might be pierced with a needle. Patients would protrude their tongues and not flinch when pierced by the needle.
- Catalepsy (waxy flexibility):
State of continual and most unusual muscular tension.
Ex: If one attempts to bend the patient’s arm, it is as if one were bending a length of thick metal wire, like soldering wire. The remarkable aspect here is that, as in bending the wire, the patient retains whatever position the limb, or for that matter, the body, is placed in.
This symptom, rarely seen in modern times, was common before the advent of antipsychotic medicines in the middle of the twentieth century.
- Stereotypies:
bizarre, perseverated behaviors.
Ex: patient may march back and forth along the same line for hours; another may repeatedly dress and undress. Other persons may be approached again and again, each time being asked the same question. The same piece of paper may be folded and unfolded until it disintegrates. Most patients can offer no reason for their senseless activity. When asked, a patient replied, “it must be so.”
- Echolalia and echopraxia:
patient’s behavior mirrors that of the other person, and, importantly, when this happens automatically, and in the absence of any request.
If asked a question the echolalic patient will simply repeat it, sometimes over and over again.
The echopraxic patient may clumsily mirror the gestures and posture of the interviewer and, as in echolalia, may continue to do this long after the other person has left, as if uncontrollably compelled to maintain the same activity.
* Bizarre behavior:
- Mannerisms:
bizarre or odd caricatures of gestures, speech, or behavior.
Ex: In manneristic gesturing- patients may offer their hands to shake with the fingers splayed out, or the fingers may writhe in a peculiar, contorted way.
In manneristic speech- cadence, modulation, or volume are erratic and dysmodulated. One patient may speak in a singsong voice, another in a telegraphic style, and yet another with pompous accenting of random syllables.
In manneristic behavior- rather than walking, some patients may march in bizarre, stiff-legged fashion.
- Bizarre affect:
represent a distortion of the normal connection between felt emotion and affective expression.
facial expression appears theatrical, wooden, or under a peculiar constraint.
Patients may report feeling joy, yet the rapturous facial expression may appear brittle and tenuous.
Conversely patients may report grief, and indeed tears may be present, yet the emotion lacks depth, as if patients were merely wearing a mask of grief that might disappear at any moment.
Another, very important form of bizarre affect is unprovoked and mirthless laughter. For no apparent reason patients may break into bizarre and unrestrainable laughter. Though appearing neither happy nor amused, the laughter continues.
- Inappropriate affect may also be seen:
Here the connection between the patient’s ideas and affect seems completely severed.
A young patient, grief stricken at a parent’s funeral, was seen to snicker; another patient, relating the infernal tortures suffered just the night before, smiled beatifically.
- Deterioration of behavior:
Patients become untidy and may neglect to bathe or wash their clothes; the fingernails may become very long. Dress and grooming may become bizarre. Several layers of clothing are often worn, even during the summer. Bits of string or cloth may festoon the patient’s hair or garments; makeup may be smeared on.
Not uncommonly, paranoid patients shave their heads, and this often reliably predicts an oncoming
exacerbation of illness, and also some form of selfmutilation.
Patients may pluck out their eyelashes or cut deep gouges in their legs.
Some seem to be almost completely analgesic: an eye may be plucked out; pieces of flesh may be
bitten off; in extreme cases, self-evisceration may occur, “just to see” what the intestines look like.
* Negative symptoms:
- Flattening of affect (when less severe- “blunting” of affect)
Characterized by a lifeless and wooden facial expression accompanied by an absence or diminution of all feelings.
This is quite different from a depressed appearance. In depression patients appear drained or weighted down; there is a definite sense of something there.
In flattening, however, patients seem to have nothing to express; they are simply devoid of emotion. They appear unmoved, wooden, and almost at times as if they were machines.
Poverty of speech:
patients, though perhaps talking a normal amount, seem to “say” very little.
There is a dearth of meaningful content to what they say and speech is often composed of stock phrases and repetitions.
Poverty of thought:
characterized by a far-reaching impoverishment of the entire thinking of the patient.
patient may complain of having “no thoughts,” that “the head is empty,” that there are no “stirrings.” Of its own accord nothing “comes to mind.”
If pressed by a question the patient may offer a sparse reply, then fail to say anything else.
Avolition (referred to by Kraepelin as “annihilation of the will”):
It is said to be present when patients have lost the capacity to embark on almost any goal-directed activity.
Ex: Bills are not paid; the house is not cleaned; infants are neither changed nor fed. This is not because patients feel inhibited, lack interest, or suffer from fatigue, but rather because the ability to will an action has become deficient.
Ambivalence:
may render patients incapable of almost any volitional activity.
Here, patients experience two opposed courses of action at the same time, and for lack of ability to decide between them, do nothing.
Ex: One patient stood at the washstand for hours unable to decide whether to shave or to use the toothbrush.
This “paralysis of will,” however, may at times be easily removed if another person gives directions. In
this case an aide simply told the patient to brush his teeth and then put the toothbrush in the patient’s hand. Immediately and with peculiar alacrity the patient then set to brushing his teeth.
Imp- This kind of ambivalence found in schizophrenia is to be distinguished from the indecisiveness seen at times in depression and the “normal” ambivalence that anyone may experience.
The depressed patient’s inability to embark on decision-making stems more from a lack of energy and
initiative; unlike the patient with schizophrenia, the depressed patient generally is not able to act when others make the decision.
In normal circumstances competing desires may leave the patient unable to decide. With time, however, a normal person makes a decision because the capacity to do so is not lost. In schizophrenia, however, it is this very capacity that is no longer present.
“Double bookkeeping” :
refers to the patient’s ability to, as it were, live in two worlds at the same time.
On the one hand is the world of voices, visions, and delusions, and on the other hand, and quite coincident with this psychotic world, is the world as perceived by others. To the patient both worlds seem quite real.
Ex: a patient may hear a voice as clearly as the voice of the physician and believe it just as real, yet at the same time acknowledge that the physician does not hear it.
Or the grandiose patient who fully believed that a coronation was imminent may yet continue to work at a janitor’s job and go on doing so, living in two worlds, and feeling little if any conflict between them.
A variant of double bookkeeping, known as “double orientation,” or “delusional disorientation,” may at times mislead the interviewer into thinking that the patient is disoriented.
Ex: grandiose patient believed that he was John F. Kennedy, and when asked what year it was replied 1962. Later on, however, when filling out a form, he put down the correct year.
Last edited by Admin on Sun May 20, 2012 3:38 pm; edited 3 times in total
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
3. Schizophrenia Subtypes:
Paranoid type
A type of schizophrenia in which the following criteria are met:
(a) Preoccupation with one or more delusions or frequent auditory hallucinations.
(b) None of the following is prominent:
- Disorganized speech
- Disorganized or catatonic behavior, or
- Flat or inappropriate affect.
tends to have a later onset than the other subtypes.
In paranoid schizophrenia, more so than in the other subtypes, the delusions may be somewhat systematized (a group of delusions organized around a common theme), even plausible.
In most cases, however, inconsistencies appear, which, however, have no impact on the patients.
Catatonic type
Presence of at least two of the following:
(a) motoric immobility as evidenced by catalepsy (including waxy flexibility) or stupor
(b) excessive motor activity (that is apparently purposeless and not influenced by external stimuli)
(c) extreme negativism (an apparently motiveless resistance to all instructions or maintenance of a rigid posture against attempts to be moved) or mutism
(d) peculiarities of voluntary movement as evidenced by posturing (voluntary assumption of inappropriate or bizarre postures), stereotyped movements, prominent mannerisms, or prominent grimacing
(e) echolalia or echopraxia
manifests in one of two forms: stuporous catatonia or excited catatonia.
Stuporous form:
one sees varying combinations of immobility, negativism, mutism, posturing, and waxy flexibility.
Ex: One patient curled into a rigid ball and lay on the bed, unspeaking, for days, moving neither for defecation nor urination, and catheterization was eventually required. Saliva drooled from the mouth, and as there was no chewing, food simply lay in the oral cavity and there was danger of aspiration. Another patient stood praying in a corner, mumbling very softly. A degree of waxy flexibility was present, and the patient’s arm would, for a time, remain in any position it was placed, only
eventually to slowly return to the position of prayer.
Excited form of catatonia:
One may see purposeless, senseless, frenzied activity, multiple stereotypies, and at times extreme impulsivity.
Patients may scream, howl, beat their sides repeatedly, jump up, hop about, or skitter back and forth.
Ex: A patient leaped up and attacked a bystander for no reason, then immediately returned to a corner and restlessly marched in place, squeaking loudly. Often speech is extremely stereotyped and bizarre. Patients may shout, declaim, preach, and pontificate in an incoherent fashion. Words and phrases may be repeated hundreds of times.
Typically, despite their extreme activity, these patients remain for the most part withdrawn. They often make little or no effort to interact with others; they keep their excitation to themselves, perhaps in a corner, perhaps under a bed.
Although some patients with catatonic schizophrenia may display only one of these two forms, in most cases they are seen to alternate in the same patient.
Disorganized type (hebephrenic)
All of the following are prominent:
(a) disorganized speech
(b) disorganized behavior
(c) flat or inappropriate affect
(d) The criteria are not met for catatonic type.
have an earlier onset than the other subtypes and tends to develop very insidiously.
Overall the behavior of these patients seems at times a caricature of childish silliness. Senselessly
they may busy themselves first with this, then with that, generally to no purpose, and often with silly, shallow laughter.
Delusions, when they occur, are unsystematized and often hypochondriacal in nature.
Some may display very marked loosening of associations to the point of a fatuous, almost driveling incoherence.
Undifferentiated type
A type of schizophrenia in which symptoms that meet Criterion A are present, but the criteria are not met for the paranoid, disorganized, or catatonic type.
In some instances the clinical picture, which initially did “fit” a subtype description, may gradually change such that it no longer squares with one of the specific subtypes: this appears to be more common with the catatonic and hebephrenic subtypes than with paranoid or simple schizophrenia.
Simple schizophrenia
has perhaps the earliest age of onset, often first beginning in childhood, and
shows very gradual and insidious progression over many years.
Delusions, hallucinations, and loosening of associations are sparse, and indeed are for the most part absent.
Rather the clinical picture is dominated by the annihilation of the will, impoverishment of thought, and flattening of affect.
Gradually over the years these patients fall away from their former goals and often become cold and distant with their former acquaintances.
They may appear shiftless, and some are accused of laziness.
Few thoughts disturb their days, and they may seem quite content to lie in bed or sit in a darkened room all day.
For the most part, however, these patients do little to attract any attention; some continue to live with aged parents; others pass from one homeless mission to another.
HY Facts:
- Those with paranoid or catatonic schizophrenia tend to pursue a fluctuating course, and of the two the eventual outcome appears to be worse for the catatonic subtype.
- The hebephrenic and simple subtypes tend to pursue either a stable or progressively deteriorating
chronicity, and of the two the simple subtype seems to often undergo the greatest deterioration.
Schizophrenia can also be divided into Type I/Good prognosis and Type II/Poor prognosis
Paranoid type
A type of schizophrenia in which the following criteria are met:
(a) Preoccupation with one or more delusions or frequent auditory hallucinations.
(b) None of the following is prominent:
- Disorganized speech
- Disorganized or catatonic behavior, or
- Flat or inappropriate affect.
tends to have a later onset than the other subtypes.
In paranoid schizophrenia, more so than in the other subtypes, the delusions may be somewhat systematized (a group of delusions organized around a common theme), even plausible.
In most cases, however, inconsistencies appear, which, however, have no impact on the patients.
Catatonic type
Presence of at least two of the following:
(a) motoric immobility as evidenced by catalepsy (including waxy flexibility) or stupor
(b) excessive motor activity (that is apparently purposeless and not influenced by external stimuli)
(c) extreme negativism (an apparently motiveless resistance to all instructions or maintenance of a rigid posture against attempts to be moved) or mutism
(d) peculiarities of voluntary movement as evidenced by posturing (voluntary assumption of inappropriate or bizarre postures), stereotyped movements, prominent mannerisms, or prominent grimacing
(e) echolalia or echopraxia
manifests in one of two forms: stuporous catatonia or excited catatonia.
Stuporous form:
one sees varying combinations of immobility, negativism, mutism, posturing, and waxy flexibility.
Ex: One patient curled into a rigid ball and lay on the bed, unspeaking, for days, moving neither for defecation nor urination, and catheterization was eventually required. Saliva drooled from the mouth, and as there was no chewing, food simply lay in the oral cavity and there was danger of aspiration. Another patient stood praying in a corner, mumbling very softly. A degree of waxy flexibility was present, and the patient’s arm would, for a time, remain in any position it was placed, only
eventually to slowly return to the position of prayer.
Excited form of catatonia:
One may see purposeless, senseless, frenzied activity, multiple stereotypies, and at times extreme impulsivity.
Patients may scream, howl, beat their sides repeatedly, jump up, hop about, or skitter back and forth.
Ex: A patient leaped up and attacked a bystander for no reason, then immediately returned to a corner and restlessly marched in place, squeaking loudly. Often speech is extremely stereotyped and bizarre. Patients may shout, declaim, preach, and pontificate in an incoherent fashion. Words and phrases may be repeated hundreds of times.
Typically, despite their extreme activity, these patients remain for the most part withdrawn. They often make little or no effort to interact with others; they keep their excitation to themselves, perhaps in a corner, perhaps under a bed.
Although some patients with catatonic schizophrenia may display only one of these two forms, in most cases they are seen to alternate in the same patient.
Disorganized type (hebephrenic)
All of the following are prominent:
(a) disorganized speech
(b) disorganized behavior
(c) flat or inappropriate affect
(d) The criteria are not met for catatonic type.
have an earlier onset than the other subtypes and tends to develop very insidiously.
Overall the behavior of these patients seems at times a caricature of childish silliness. Senselessly
they may busy themselves first with this, then with that, generally to no purpose, and often with silly, shallow laughter.
Delusions, when they occur, are unsystematized and often hypochondriacal in nature.
Some may display very marked loosening of associations to the point of a fatuous, almost driveling incoherence.
Undifferentiated type
A type of schizophrenia in which symptoms that meet Criterion A are present, but the criteria are not met for the paranoid, disorganized, or catatonic type.
In some instances the clinical picture, which initially did “fit” a subtype description, may gradually change such that it no longer squares with one of the specific subtypes: this appears to be more common with the catatonic and hebephrenic subtypes than with paranoid or simple schizophrenia.
Simple schizophrenia
has perhaps the earliest age of onset, often first beginning in childhood, and
shows very gradual and insidious progression over many years.
Delusions, hallucinations, and loosening of associations are sparse, and indeed are for the most part absent.
Rather the clinical picture is dominated by the annihilation of the will, impoverishment of thought, and flattening of affect.
Gradually over the years these patients fall away from their former goals and often become cold and distant with their former acquaintances.
They may appear shiftless, and some are accused of laziness.
Few thoughts disturb their days, and they may seem quite content to lie in bed or sit in a darkened room all day.
For the most part, however, these patients do little to attract any attention; some continue to live with aged parents; others pass from one homeless mission to another.
HY Facts:
- Those with paranoid or catatonic schizophrenia tend to pursue a fluctuating course, and of the two the eventual outcome appears to be worse for the catatonic subtype.
- The hebephrenic and simple subtypes tend to pursue either a stable or progressively deteriorating
chronicity, and of the two the simple subtype seems to often undergo the greatest deterioration.
Schizophrenia can also be divided into Type I/Good prognosis and Type II/Poor prognosis
| Type I Schizophrenia | Type II Schizophrenia | |
| Premorbid personality | Normal | Poor adjustment |
| Age of onset | Late, often adult years | Early |
| Mode of onset | Acute | Gradual and insidious |
| Premorbid social, sexual, and work histories | Good | Poor |
| Kind of symptoms | Positive | Negative |
| Marital Status | Married | Single, divorced, or widowed |
| Family history of | mood disorders | schizophrenia |
| support systems | Good | Poor |
| Ventriculomegaly on CT scan | Absent | Present |
| Prognosis | Good | Poor |
Last edited by Admin on Sun May 20, 2012 3:42 pm; edited 2 times in total
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
4. Neuroanatomy Changes: First Episode vs Chronic Schizophrenia
Meta-Analysis published by Ellison-Wright, Glahn and Laird et al to map gray matter changes in first-episode schizophrenia and to compare these with the changes in chronic schizophrenia.
Results of the Meta-Analysis:

Source: Am J Psychiatry
- CT and MRI scans have conclusively demonstrated ventricular dilitation and cortical atrophy in schizophrenia
- There is a good correlation between the degree of atrophy of the posterior portion of the left superior temporal gyrus and the severity of auditory hallucinations and speech disorganization.
- Some studies have also demonstrated atrophy of the thalamus; however, these findings are not as robust.
- Enlargement of the basal ganglia, demonstrated in earlier studies, now appears to be an artifact of antipsychotic treatment.
- Interestingly, the ventricular dilitation and cortical atrophy are present at the onset of the disease, and some studies have also suggested that they may progressively worsen over time.
Check the following Diagrams to better understand the Neuroanatomy:



*** Please Add Your Comments on This Article. ****
Meta-Analysis published by Ellison-Wright, Glahn and Laird et al to map gray matter changes in first-episode schizophrenia and to compare these with the changes in chronic schizophrenia.
Results of the Meta-Analysis:

Source: Am J Psychiatry
- CT and MRI scans have conclusively demonstrated ventricular dilitation and cortical atrophy in schizophrenia
- There is a good correlation between the degree of atrophy of the posterior portion of the left superior temporal gyrus and the severity of auditory hallucinations and speech disorganization.
- Some studies have also demonstrated atrophy of the thalamus; however, these findings are not as robust.
- Enlargement of the basal ganglia, demonstrated in earlier studies, now appears to be an artifact of antipsychotic treatment.
- Interestingly, the ventricular dilitation and cortical atrophy are present at the onset of the disease, and some studies have also suggested that they may progressively worsen over time.
Check the following Diagrams to better understand the Neuroanatomy:



*** Please Add Your Comments on This Article. ****
Last edited by Admin on Sat Nov 21, 2015 11:54 pm; edited 1 time in total
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
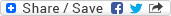
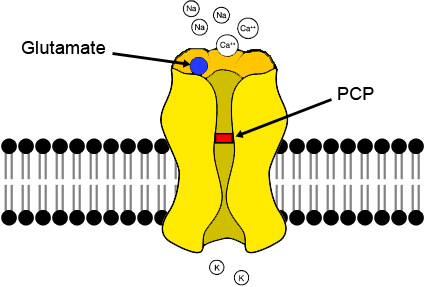
5. Phencyclidine Model of Schizophrenia
Schizophrenia is characterized by deficits in cognition known to be dependent upon the functional integrity of the prefrontal cortex (PFC).
While the pathophysiological basis of PFC dysfunction in schizophrenia is not completely understood, a central role for NMDA receptor hypofunction is widely supported. For example, subchronic exposure to the NMDA receptor antagonist phencyclidine (PCP) induces cognitive deficits and a ‘hypofrontality’ which directly parallels that seen in schizophrenia [1-3].
Furthermore, sub-chronic PCP exposure induces alterations in GABAergic cell markers and 5-HT receptor expression in the PFC similar to those seen in this disorder [1,4,5]. Subchronic exposure to PCP produces a persistent decrease in dopamine utilization within the prefrontal cortex, which is accompanied by a deficit in working memory in prefrontal cortex-dependent tasks in both rats (6) and nonhuman primates (7). These findings have been reviewed by Jentsch and Roth ( 8 ) as supporting NMDA receptor antagonist models of schizophrenia.
While this evidence places NMDA receptor hypofunction central to the pathophysiology of PFC dysfunction in schizophrenia, the mechanisms through which NMDA hypofunction promotes PFC dysfunction are poorly understood.
PCP and its congener, ketamine, have been shown to induce a psychosis in humans that closely resembles schizophrenia and is representative of both the negative and positive symptoms of the disease, and also to exacerbate symptoms in chronic stabilized schizophrenic patients (9-12).
Animal studies have demonstrated that acute treatment with PCP gives rise to an array of symptoms that relate to schizophrenia, including cognitive deficits (6,7,13,14), disruption in sensory motor gating (15) and impaired social interaction (16).
Furthermore, it has been demonstrated that some effects of NMDA receptor antagonists (such as neurotoxicity) in rats are age dependent (17,18), which reflects a similar scenario in humans in relation to the onset of sensitivity to the psychotomimetic effects of ketamine (19) and the symptoms of schizophrenia.
Numerous human imaging studies have employed positron emission tomography in schizophrenic patients, either to measure cerebral blood flow or else to measure local cerebral glucose utilization, which is directly related to neuronal activity, with [18F] fluorodeoxyglucose (FDGPET). These studies have frequently revealed an absolute or relative metabolic hypofunction within particular brain areas that have been shown to have altered neuropathology and neurochemical deficits in schizophrenia (Hazlett et al, 2000; Buchsbaum and Hazlett, 1998; Cohen et al, 1997; Buchsbaum et al, 1996; Nordahl et al, 1996; Schroder et al, 1996, 1994; Potkin et al, 1994; Wolkin et al, 1992; Andreasen et al, 1992; Tamminga et al, 1992; Buchsbaum et al, 1990).
In particular, the altered metabolic activity in the prefrontal cortex in the schizophrenic brain has been shown to correlate with the presence and severity of negative symptoms and cognitive deficits (Hazlett et al, 2000; Volz et al, 1999; Buchsbaum and Hazlett, 1998; Schroder et al, 1996; Schroeder et al, 1994; Wolkin et al, 1992; Tamminga et al, 1992; Andreasen et al, 1992; Buchsbaum et al, 1990), while altered metabolic activities within the temporal lobe and thalamus have been shown to correlate with positive symptomology (Buchsbaum and Hazlett, 1998; Buchsbaum et al, 1996; Nordahl et al, 1996; Schroder et al, 1996; Tamminga et al, 1992).
Moreover, chronic exposure to PCP in humans has been shown to produce a metabolic hypofunction during frontal activation tasks (Wu et al, 1991), similar to that observed in schizophrenia, and to produce enduring cognitive deficits (Cosgrove and Newell, 1991). Strikingly, however, chronic PCP treatment has never been shown to produce a neuroanatomical pattern of hypofunction in rodents, which mirrors that observed in schizophrenic patients.
REFERENCES:
1. Cochran SM, Kennedy M, McKerchar CE, Steward LJ, Pratt JA, Morris BJ: Induction of Metabolic Hypofunction and Neurochemical Deficits after Chronic Intermittent Exposure to Phencyclidine: Differential Modulation by Antipsychotic Drugs. Neuropsychopharmacology 2003, 28:265-275.
2. Dawson N, Thompson RJ, McVie A, Thomson DM, Morris BJ, Pratt JA: Modafinil reverses phencyclidine (PCP)-induced deficits in cognitive flexibility, cerebral metabolism and functional brain connectivity. Schizophrenia Bulletin .
3. Egerton A, Reid L, McGregor S, Cochran SM, Morris BJ, Pratt JA: Subchronic and chronic PCP treatment produces temporally distinct deficits in attentional set shifting and prepulse inhibition in rats. Psychopharmacology 2008, 198:37-49.
4. Egerton A, Reid L, McKerchar CE, Morris BJ, Pratt JA: Impairment in perceptual attentional set-shifting following PCP administration: a rodent model of set-shifting deficits in schizophrenia.
Psychopharmacology 2005, 179:77-84.
5. Steward LJ, Kennedy MD, Morris BJ, Pratt JA: The atypical antipsychotic drug clozapine enhances chronic PCP-induced regulation of prefrontal cortex 5-HT2A receptors. Neuropharmacology 2004, 47:527-537.
6. Jentsch JD, Redmond DE, Elsworth JD, Taylor JR, Youngren KD, Roth RH (1997a). Enduring cognitive deficits and cortical dopamine dysfunction in monkeys after long-term administration of phencyclidine. Science 277: 953–955.
7. Jentsch JD, Tran A, Le D, Youngren KD, Roth RH (1997b). Subchronic phencyclidine administration reduces mesoprefrontal dopamine utilization and impairs prefrontal corticaldependent cognition in the rat. Neuropsychopharmacology 17: 92–99.
8. Jentsch JD, Roth RH (1999). The Neuropsychopharmacology of Phencyclidine: from NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia. Neuropsychopharmacology 20: 201–225.
9. Luby ED, Cohen CB, Rosenbaum G, Gottlieb JS, Kelly R (1959). Study of a new schizophrenomimetic drug FSerynl. Arch Neurol Psychiatry 81: 363–369.
10. Allen RM, Young SJ (1978). Phencyclidine-induced psychosis. Am J Psychiatry 135: 1081–1084.
11. Javitt DC, Zukin SR (1991). Recent advances in the phencyclidine model of schizophrenia. AM J Psychiatry 148: 1301–1308.
12. Krystal JH, Karper LP, Seibyl JP, Freeman GK, Delaney R, Bremner JD et al (1994). Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry 51: 199–214.
13. Adams B, Moghaddam B (1998). Corticolimbic dopamine neurotransmission is temporally dissociated from the cognitive and locomotor effects of phencyclidine. J Neurosci 18: 5545–5554.
14. Kesner RP, Dakis M (1997). Intrahippocampal injections of phencyclidine but not naloxone disrupt acquisition of a spatial continuous recognition memory task. Pharmacol Biochem Behav 56: 97–101.
15. Mansbach RS, Geyer MA (1989). Effects of phencyclidine and phencyclidine biologs on sensorimotor gating in the rat. Neuropsychopharmacology 2: 299–308.
16. Sams-Dodd F (1997). Effect of novel antipsychotic drugs on phencyclidine-induced stereotyped behaviour and social isolation in the rat social interaction test. Behav Pharmacol 8: 196–215.
17. Farber NB, Wozniak DF, Price MT, Labruyere J, Huss J, St Peter H et al (1995). Age-specific neurotoxicity in the rat associated with NMDA receptor blockade: potential relevance to schizophrenia?
Biol Psychiatry 38: 788–796.
18. Olney JW, Farber NB (1995). Glutamate receptor dysfunction and schizophrenia. Arch Gen Psychiatry 52: 998–1007.
19. Reich DL, Silvay G (1989). Ketamine: an update on the first twenty-five years of clinical experience. Can J Anaesth 36: 186–197.
Schizophrenia is characterized by deficits in cognition known to be dependent upon the functional integrity of the prefrontal cortex (PFC).
While the pathophysiological basis of PFC dysfunction in schizophrenia is not completely understood, a central role for NMDA receptor hypofunction is widely supported. For example, subchronic exposure to the NMDA receptor antagonist phencyclidine (PCP) induces cognitive deficits and a ‘hypofrontality’ which directly parallels that seen in schizophrenia [1-3].
Furthermore, sub-chronic PCP exposure induces alterations in GABAergic cell markers and 5-HT receptor expression in the PFC similar to those seen in this disorder [1,4,5]. Subchronic exposure to PCP produces a persistent decrease in dopamine utilization within the prefrontal cortex, which is accompanied by a deficit in working memory in prefrontal cortex-dependent tasks in both rats (6) and nonhuman primates (7). These findings have been reviewed by Jentsch and Roth ( 8 ) as supporting NMDA receptor antagonist models of schizophrenia.
While this evidence places NMDA receptor hypofunction central to the pathophysiology of PFC dysfunction in schizophrenia, the mechanisms through which NMDA hypofunction promotes PFC dysfunction are poorly understood.
PCP and its congener, ketamine, have been shown to induce a psychosis in humans that closely resembles schizophrenia and is representative of both the negative and positive symptoms of the disease, and also to exacerbate symptoms in chronic stabilized schizophrenic patients (9-12).
Animal studies have demonstrated that acute treatment with PCP gives rise to an array of symptoms that relate to schizophrenia, including cognitive deficits (6,7,13,14), disruption in sensory motor gating (15) and impaired social interaction (16).
Furthermore, it has been demonstrated that some effects of NMDA receptor antagonists (such as neurotoxicity) in rats are age dependent (17,18), which reflects a similar scenario in humans in relation to the onset of sensitivity to the psychotomimetic effects of ketamine (19) and the symptoms of schizophrenia.
Numerous human imaging studies have employed positron emission tomography in schizophrenic patients, either to measure cerebral blood flow or else to measure local cerebral glucose utilization, which is directly related to neuronal activity, with [18F] fluorodeoxyglucose (FDGPET). These studies have frequently revealed an absolute or relative metabolic hypofunction within particular brain areas that have been shown to have altered neuropathology and neurochemical deficits in schizophrenia (Hazlett et al, 2000; Buchsbaum and Hazlett, 1998; Cohen et al, 1997; Buchsbaum et al, 1996; Nordahl et al, 1996; Schroder et al, 1996, 1994; Potkin et al, 1994; Wolkin et al, 1992; Andreasen et al, 1992; Tamminga et al, 1992; Buchsbaum et al, 1990).
In particular, the altered metabolic activity in the prefrontal cortex in the schizophrenic brain has been shown to correlate with the presence and severity of negative symptoms and cognitive deficits (Hazlett et al, 2000; Volz et al, 1999; Buchsbaum and Hazlett, 1998; Schroder et al, 1996; Schroeder et al, 1994; Wolkin et al, 1992; Tamminga et al, 1992; Andreasen et al, 1992; Buchsbaum et al, 1990), while altered metabolic activities within the temporal lobe and thalamus have been shown to correlate with positive symptomology (Buchsbaum and Hazlett, 1998; Buchsbaum et al, 1996; Nordahl et al, 1996; Schroder et al, 1996; Tamminga et al, 1992).
Moreover, chronic exposure to PCP in humans has been shown to produce a metabolic hypofunction during frontal activation tasks (Wu et al, 1991), similar to that observed in schizophrenia, and to produce enduring cognitive deficits (Cosgrove and Newell, 1991). Strikingly, however, chronic PCP treatment has never been shown to produce a neuroanatomical pattern of hypofunction in rodents, which mirrors that observed in schizophrenic patients.
REFERENCES:
1. Cochran SM, Kennedy M, McKerchar CE, Steward LJ, Pratt JA, Morris BJ: Induction of Metabolic Hypofunction and Neurochemical Deficits after Chronic Intermittent Exposure to Phencyclidine: Differential Modulation by Antipsychotic Drugs. Neuropsychopharmacology 2003, 28:265-275.
2. Dawson N, Thompson RJ, McVie A, Thomson DM, Morris BJ, Pratt JA: Modafinil reverses phencyclidine (PCP)-induced deficits in cognitive flexibility, cerebral metabolism and functional brain connectivity. Schizophrenia Bulletin .
3. Egerton A, Reid L, McGregor S, Cochran SM, Morris BJ, Pratt JA: Subchronic and chronic PCP treatment produces temporally distinct deficits in attentional set shifting and prepulse inhibition in rats. Psychopharmacology 2008, 198:37-49.
4. Egerton A, Reid L, McKerchar CE, Morris BJ, Pratt JA: Impairment in perceptual attentional set-shifting following PCP administration: a rodent model of set-shifting deficits in schizophrenia.
Psychopharmacology 2005, 179:77-84.
5. Steward LJ, Kennedy MD, Morris BJ, Pratt JA: The atypical antipsychotic drug clozapine enhances chronic PCP-induced regulation of prefrontal cortex 5-HT2A receptors. Neuropharmacology 2004, 47:527-537.
6. Jentsch JD, Redmond DE, Elsworth JD, Taylor JR, Youngren KD, Roth RH (1997a). Enduring cognitive deficits and cortical dopamine dysfunction in monkeys after long-term administration of phencyclidine. Science 277: 953–955.
7. Jentsch JD, Tran A, Le D, Youngren KD, Roth RH (1997b). Subchronic phencyclidine administration reduces mesoprefrontal dopamine utilization and impairs prefrontal corticaldependent cognition in the rat. Neuropsychopharmacology 17: 92–99.
8. Jentsch JD, Roth RH (1999). The Neuropsychopharmacology of Phencyclidine: from NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia. Neuropsychopharmacology 20: 201–225.
9. Luby ED, Cohen CB, Rosenbaum G, Gottlieb JS, Kelly R (1959). Study of a new schizophrenomimetic drug FSerynl. Arch Neurol Psychiatry 81: 363–369.
10. Allen RM, Young SJ (1978). Phencyclidine-induced psychosis. Am J Psychiatry 135: 1081–1084.
11. Javitt DC, Zukin SR (1991). Recent advances in the phencyclidine model of schizophrenia. AM J Psychiatry 148: 1301–1308.
12. Krystal JH, Karper LP, Seibyl JP, Freeman GK, Delaney R, Bremner JD et al (1994). Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry 51: 199–214.
13. Adams B, Moghaddam B (1998). Corticolimbic dopamine neurotransmission is temporally dissociated from the cognitive and locomotor effects of phencyclidine. J Neurosci 18: 5545–5554.
14. Kesner RP, Dakis M (1997). Intrahippocampal injections of phencyclidine but not naloxone disrupt acquisition of a spatial continuous recognition memory task. Pharmacol Biochem Behav 56: 97–101.
15. Mansbach RS, Geyer MA (1989). Effects of phencyclidine and phencyclidine biologs on sensorimotor gating in the rat. Neuropsychopharmacology 2: 299–308.
16. Sams-Dodd F (1997). Effect of novel antipsychotic drugs on phencyclidine-induced stereotyped behaviour and social isolation in the rat social interaction test. Behav Pharmacol 8: 196–215.
17. Farber NB, Wozniak DF, Price MT, Labruyere J, Huss J, St Peter H et al (1995). Age-specific neurotoxicity in the rat associated with NMDA receptor blockade: potential relevance to schizophrenia?
Biol Psychiatry 38: 788–796.
18. Olney JW, Farber NB (1995). Glutamate receptor dysfunction and schizophrenia. Arch Gen Psychiatry 52: 998–1007.
19. Reich DL, Silvay G (1989). Ketamine: an update on the first twenty-five years of clinical experience. Can J Anaesth 36: 186–197.
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
6. Differential Diagnosis:
1. Manic Episode (Bipolar Disorder):
2. Depressive Episodes (MDD or Bipolar Disorder):
3. Alcohol hallucinosis or Alcoholic paranoia:
- Difficult to differentiate between alcohol hallucinosis or alcoholic paranoia and schizophrenia.
- Presence of mannerisms, stereotypies, or loosened associations favor schizophrenia
- Remission of symptoms after 6 months or more of abstinence would favor alcohol hallucinosis or alcoholic paranoia.
4. Paranoid Personality Disorder
5. Schizoid Personality Disorder
6. Schizotypal Personality Disorder
7. Autism:
8. Delusional Disorder:
1. Manic Episode (Bipolar Disorder):
| Bipolar Disorder | Schizophrenia | |
| Course | Psychotic symptoms almost always precede the excitation (Chronic Illness) | Affective symptoms appear first, and psychotic ones only appear as the patient progresses into the acute stage of mania (episodic illness) |
| Mood & Affect | The mood and affect of a patient with mania are typically “infectious” and well developed | mood of an excited hebephrenic is one of silly, shallow hilarity, which, rather than provoking laughter, might leave the interviewer with a sense of puzzlement |
| Activity of patient | outgoing and extroverted | though hyperactive, remains withdrawn and may actually avoid contact with others |
| When Agitated | “on the attack” | “on guard” |
2. Depressive Episodes (MDD or Bipolar Disorder):
| Depressive Episodes | Schizophrenia | |
| Psychotic symptoms | Psychotic symptoms are preceded by the depressive ones and only occur when the depressive symptoms are severe | no invariable relationship exists between them and the psychotic symptoms. |
| Delusions | mood congruent | Bizarre & generally unrelated to the mood |
3. Alcohol hallucinosis or Alcoholic paranoia:
- Difficult to differentiate between alcohol hallucinosis or alcoholic paranoia and schizophrenia.
- Presence of mannerisms, stereotypies, or loosened associations favor schizophrenia
- Remission of symptoms after 6 months or more of abstinence would favor alcohol hallucinosis or alcoholic paranoia.
4. Paranoid Personality Disorder
| Paranoid Personality Disorder | Delusional disorder and Schizophrenia |
| Reality testing intact | Reality testing lost |
5. Schizoid Personality Disorder
| Schizoid Personality Disorder | Schizophrenia |
| Reality testing intact | Reality testing not intact |
| Abstracting ability normal | Abstracting ability impaired |
| Presence of formal thought process | formal thought process impaired |
6. Schizotypal Personality Disorder
| Schizotypal Personality Disorder | Schizophrenia |
| 1) Reality testing intact; 2) Psychosis absent | 1) Reality testing lost; 2) Psychosis present |
7. Autism:
| Autism | Schizophrenia |
| If symptoms appear before the age of 3 years, autism is the more likely diagnosis, | earliest noted age of onset of schizophrenia is 5 years of age |
| presence of hallucinations and delusions indicates schizophrenia | |
| presence of typical autistic symptoms, such as gaze avoidance or a “flapping” tremor |
8. Delusional Disorder:
| Delusional Disorder | Schizophrenia |
| Age of onset later compared to Schizophrenia | |
| Well articulated, non bizarre delusional system No hallucinations, disorganized behavior or negative symptoms | |
| Less deterioration in occupational or social functioning |
Last edited by Admin on Sun May 27, 2012 8:22 pm; edited 1 time in total
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
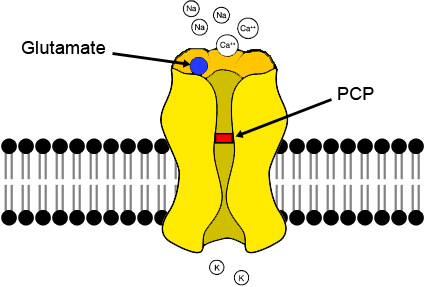
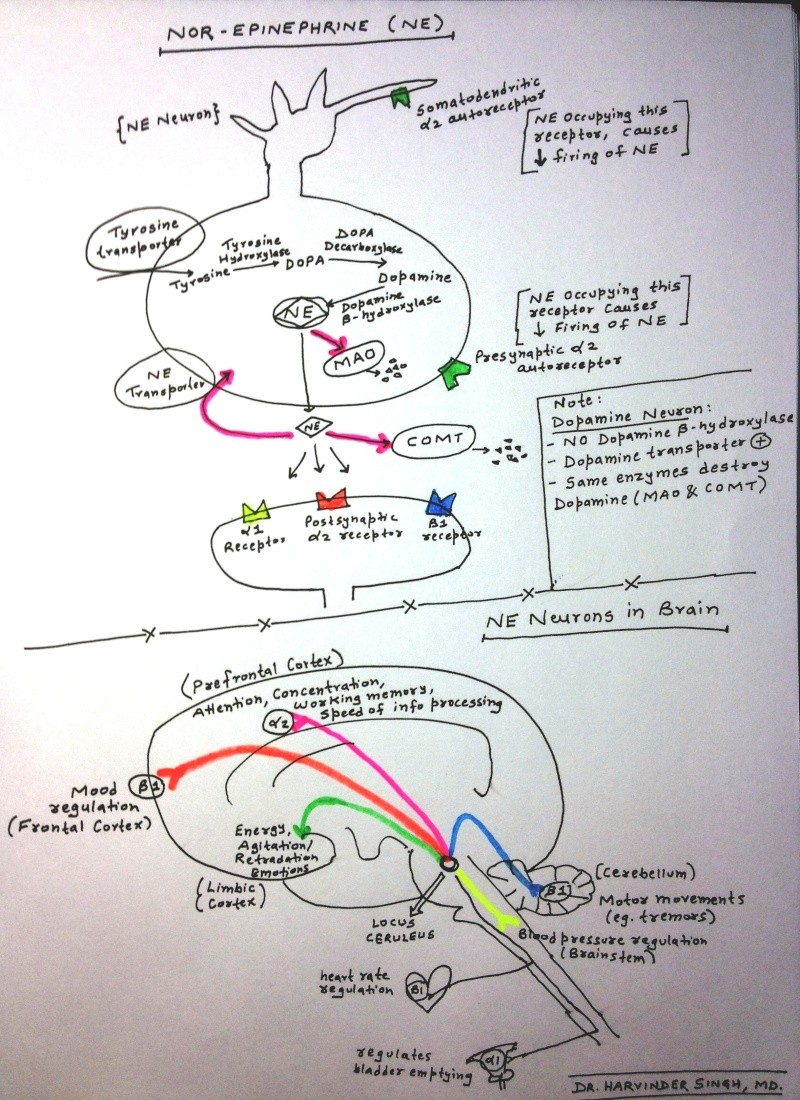
7. Role of Dopamine, Serotonin & NE Pathways in Schizophrenia:
There are four major dopaminergic pathways: mesolimbic, mesocortical, nigrostriatal, tuberoinfundibular. D2 receptors are present in all 4 pathways.
check the diagram below for Dopamine pathways explanation.
Typical antipsychotics block D2 receptors in all pathways= Mesolimbic system (decreases positive psychotic symptoms), nigrostriatal system (result in EPS), tuberoinfundibular system (causes hyperprolactinaemia)
Atypical Antipsychotics: have more effect on Seretonin (5HT2A) >>Dopamine. They block D2 receptor in mesolimbic pathway only- so no other side effects (EPS & Hyperprolactinaemia). In addition Seretonin blockage (5HT2A) increases Dopamine release in other pathways -->resulting in improvement in negative symtpoms.
Exception= Risperidone:
Risperidone has a high affinity for D2 as well as serotonin receptors. It is not "limbic specific" for the mesolimbic over the nigrostriatal tract like the other atypicals. Risperidone antagonises dopamine in the tuberoinfundibular system causing a rise in prolactin. However, its antagonist action at 5HT,sub>2A receptors in the nigrostriatal pathways may partially explain why risperidone has a low propensity to cause EPS despite its blockade of D2 receptors.
(for more details read= http://www.medsafe.govt.nz/profs/puarticles/hyperpro.htm#Atypical)
Also check below for "Basics of Nor-Epinephrine, Dopamine & Serotonin Neurons":
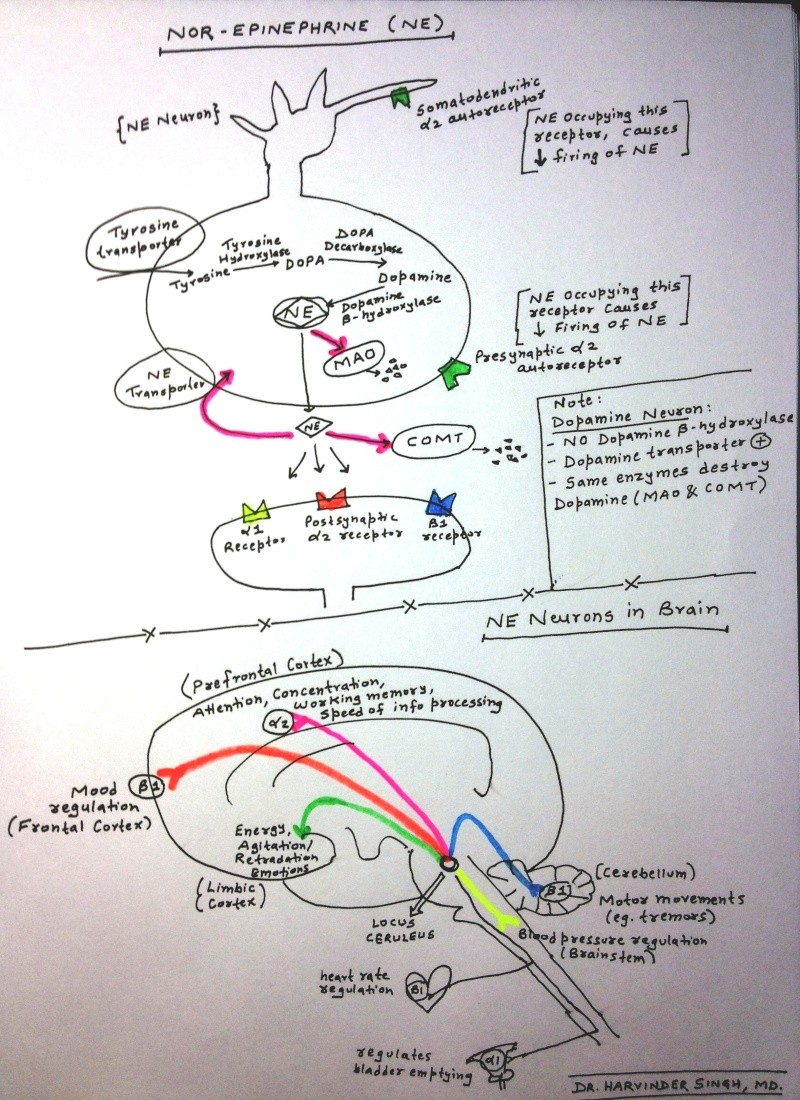

There are four major dopaminergic pathways: mesolimbic, mesocortical, nigrostriatal, tuberoinfundibular. D2 receptors are present in all 4 pathways.
check the diagram below for Dopamine pathways explanation.
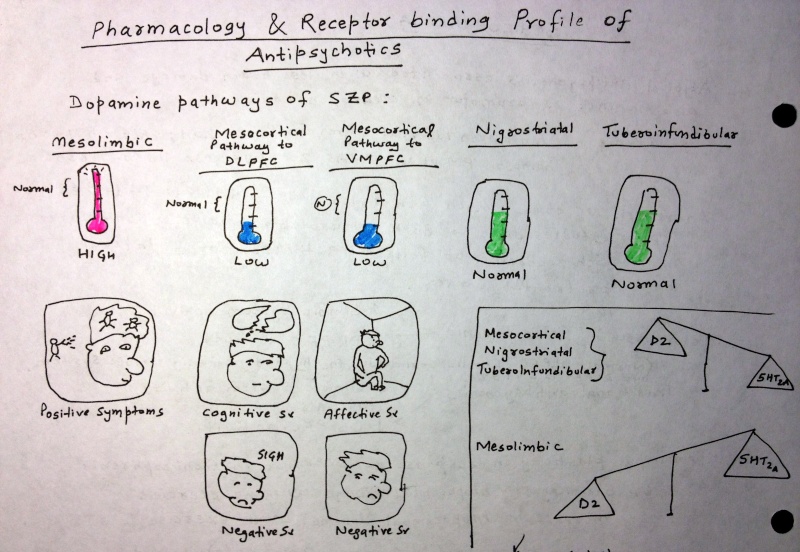
Typical antipsychotics block D2 receptors in all pathways= Mesolimbic system (decreases positive psychotic symptoms), nigrostriatal system (result in EPS), tuberoinfundibular system (causes hyperprolactinaemia)
Atypical Antipsychotics: have more effect on Seretonin (5HT2A) >>Dopamine. They block D2 receptor in mesolimbic pathway only- so no other side effects (EPS & Hyperprolactinaemia). In addition Seretonin blockage (5HT2A) increases Dopamine release in other pathways -->resulting in improvement in negative symtpoms.
Exception= Risperidone:
Risperidone has a high affinity for D2 as well as serotonin receptors. It is not "limbic specific" for the mesolimbic over the nigrostriatal tract like the other atypicals. Risperidone antagonises dopamine in the tuberoinfundibular system causing a rise in prolactin. However, its antagonist action at 5HT,sub>2A receptors in the nigrostriatal pathways may partially explain why risperidone has a low propensity to cause EPS despite its blockade of D2 receptors.
(for more details read= http://www.medsafe.govt.nz/profs/puarticles/hyperpro.htm#Atypical)
Also check below for "Basics of Nor-Epinephrine, Dopamine & Serotonin Neurons":

 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
8. Videos: Patient's View on Schizophrenia:
(a) Woman with schizophrenia tells how it feels to have this illness. This is an excerpt from an episode of Mental Health Matters, a program about mental health.
(b) Patient with Schizophrenia telling details of symptoms & course of SZP.
(c) Four patients with Schizophrenia (Case presentations):
(a) Woman with schizophrenia tells how it feels to have this illness. This is an excerpt from an episode of Mental Health Matters, a program about mental health.
(b) Patient with Schizophrenia telling details of symptoms & course of SZP.
(c) Four patients with Schizophrenia (Case presentations):
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
Post-9:
SPECIAL ARTICLE:
Research into the early course of schizophrenia has identified a prepsychotic prodromal stage (mean duration: 4.8 years) and a psychotic prephase (mean duration: 1.3 years). Comparisons of individually matched samples have demonstrated prodromal symptoms common to schizophrenia and moderate to severe depression. It is not until positive symptoms emerge that psychosis and mood disorders become
distinguishable from each other. In both disorders the prodromal stage early produces functional impairment and related social consequences.
Hence, early intervention is of great public health relevance. This intervention is targeted at manifest symptoms and not at the underlying, still unknown disease process. Cognitive-behavioural therapy at the prepsychotic prodromal stage seems to favourably influence the short-term illness course. In the psychotic prephase, a combination with low-dose antipsychotics seems to have some efficacy.
The aim of early recognition by the instruments discussed in this paper is to permit the identification of the largest possible proportion of at-risk persons as early as possible and their referral to appropriate treatment.
Find this complete article here: World Psychiatry 5:3 - October 2006
Also read this interesting article posted on "Psychiatric Times":
Q-Does an early diagnosis of schizophrenia really make a clinical difference?
By Peter F. Buckley, MD | March 1, 2012
Source: http://www.psychiatrictimes.com/display/article/10168/2041124
Early Detection of Schizophrenia: Current Evidence and Future Perspectives
HEINZ HÄFNER, KURT MAURER
Schizophrenia Research Unit, Central Institute of Mental Health, Germany

HEINZ HÄFNER, KURT MAURER
Schizophrenia Research Unit, Central Institute of Mental Health, Germany

SPECIAL ARTICLE:
Research into the early course of schizophrenia has identified a prepsychotic prodromal stage (mean duration: 4.8 years) and a psychotic prephase (mean duration: 1.3 years). Comparisons of individually matched samples have demonstrated prodromal symptoms common to schizophrenia and moderate to severe depression. It is not until positive symptoms emerge that psychosis and mood disorders become
distinguishable from each other. In both disorders the prodromal stage early produces functional impairment and related social consequences.
Hence, early intervention is of great public health relevance. This intervention is targeted at manifest symptoms and not at the underlying, still unknown disease process. Cognitive-behavioural therapy at the prepsychotic prodromal stage seems to favourably influence the short-term illness course. In the psychotic prephase, a combination with low-dose antipsychotics seems to have some efficacy.
The aim of early recognition by the instruments discussed in this paper is to permit the identification of the largest possible proportion of at-risk persons as early as possible and their referral to appropriate treatment.
Find this complete article here: World Psychiatry 5:3 - October 2006
Also read this interesting article posted on "Psychiatric Times":
Q-Does an early diagnosis of schizophrenia really make a clinical difference?
By Peter F. Buckley, MD | March 1, 2012
Source: http://www.psychiatrictimes.com/display/article/10168/2041124
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
Post-10:
Am J Psychiatry 2006; 163:600–610
Objective:
When a schizophrenia patient has an inadequate response to treatment with an antipsychotic drug, it is unclear what other antipsychotic to switch to and when to use clozapine. In this study, the authors compared switching to clozapine with switching to another atypical antipsychotic in patients who had discontinued treatment with a newer atypical antipsychotic in the context of the Clinical Antipsychotic Trials for Interventions Effectiveness (CATIE) investigation.
Method:
Ninety-nine patients who discontinued treatment with olanzapine, quetiapine, risperidone, or ziprasidone in phase 1 or 1B of the trials, primarily because of inadequate efficacy, were randomly assigned to open-label treatment with:
- Clozapine (N=49) or
- Blinded treatment with another newer atypical antipsychotic not previously received in the trial (Olanzapine [N=19], Quetiapine [N= 15], or Risperidone [N=16]).
Results:
- Time until treatment discontinuation for any reason was significantly longer for clozapine (median=10.5 months) than for quetiapine (median= 3.3), or risperidone (median=2.8 ), but not for olanzapine (median=2.7 ).
- Time to discontinuation because of inadequate therapeutic effect was significantly longer for clozapine than for olanzapine, quetiapine, or risperidone.
- At 3-month assessments, Positive and Negative Syndrome Scale total scores had decreased more in patients treated with clozapine than in patients treated with quetiapine or risperidone but not olanzapine.
- One patient treated with clozapine developed agranulocytosis, and another developed eosinophilia; both required treatment discontinuation.
Conclusions:
For these patients with schizophrenia who prospectively failed to improve with an atypical antipsychotic, clozapine was more effective than switching to another newer atypical antipsychotic. Safety monitoring is necessary to detect and manage clozapine’s serious side effects.

Effectiveness of Clozapine Versus Olanzapine, Quetiapine, and Risperidone in Patients With Chronic Schizophrenia Who Did Not Respond to Prior Atypical Antipsychotic Treatment
Am J Psychiatry 2006; 163:600–610
Objective:
When a schizophrenia patient has an inadequate response to treatment with an antipsychotic drug, it is unclear what other antipsychotic to switch to and when to use clozapine. In this study, the authors compared switching to clozapine with switching to another atypical antipsychotic in patients who had discontinued treatment with a newer atypical antipsychotic in the context of the Clinical Antipsychotic Trials for Interventions Effectiveness (CATIE) investigation.
Method:
Ninety-nine patients who discontinued treatment with olanzapine, quetiapine, risperidone, or ziprasidone in phase 1 or 1B of the trials, primarily because of inadequate efficacy, were randomly assigned to open-label treatment with:
- Clozapine (N=49) or
- Blinded treatment with another newer atypical antipsychotic not previously received in the trial (Olanzapine [N=19], Quetiapine [N= 15], or Risperidone [N=16]).
Results:
- Time until treatment discontinuation for any reason was significantly longer for clozapine (median=10.5 months) than for quetiapine (median= 3.3), or risperidone (median=2.8 ), but not for olanzapine (median=2.7 ).
- Time to discontinuation because of inadequate therapeutic effect was significantly longer for clozapine than for olanzapine, quetiapine, or risperidone.
- At 3-month assessments, Positive and Negative Syndrome Scale total scores had decreased more in patients treated with clozapine than in patients treated with quetiapine or risperidone but not olanzapine.
- One patient treated with clozapine developed agranulocytosis, and another developed eosinophilia; both required treatment discontinuation.
Conclusions:
For these patients with schizophrenia who prospectively failed to improve with an atypical antipsychotic, clozapine was more effective than switching to another newer atypical antipsychotic. Safety monitoring is necessary to detect and manage clozapine’s serious side effects.

 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
Post-11:
Context
Progressive brain volume changes in schizophrenia are thought to be due principally to the disease. However, recent animal studies indicate that antipsychotics, the mainstay of treatment for schizophrenia patients, may also contribute to brain tissue volume decrement. Because antipsychotics are prescribed for long periods for schizophrenia patients and have increasingly widespread use in other psychiatric disorders, it is imperative to determine their long-term effects on the human brain.
Objective
To evaluate relative contributions of 4 potential predictors (illness duration, antipsychotic treatment, illness severity, and substance abuse) of brain volume change.
Patients
Two hundred eleven patients with schizophrenia who underwent repeated neuroimaging beginning soon after illness onset, yielding a total of 674 high-resolution magnetic resonance scans. On average, each patient had 3 scans (≥2 and as many as 5) over 7.2 years (up to 14 years).
Main Outcome Measure
Brain volumes.
Results
- During longitudinal follow-up, antipsychotic treatment reflected national prescribing practices in 1991 through 2009.
- Longer follow-up correlated with smaller brain tissue volumes and larger cerebrospinal fluid volumes.
- Greater intensity of antipsychotic treatment was associated with indicators of generalized and specific brain tissue reduction after controlling for effects of the other 3 predictors.
- More antipsychotic treatment was associated with smaller gray matter volumes.
- Progressive decrement in white matter volume was most evident among patients who received more antipsychotic treatment.
- Illness severity had relatively modest correlations with tissue volume reduction, and alcohol/illicit drug misuse had no significant associations when effects of the other variables were adjusted.
Conclusions
Viewed together with data from animal studies, our study suggests that antipsychotics have a subtle but measurable influence on brain tissue loss over time, suggesting the importance of careful risk-benefit review of dosage and duration of treatment as well as their off-label use.
Long-term Antipsychotic Treatment and Brain Volumes:
Longitudinal Study of First-Episode Schizophrenia
Arch Gen Psychiatry. 2011;68(2):128-137
Longitudinal Study of First-Episode Schizophrenia
Arch Gen Psychiatry. 2011;68(2):128-137
Context
Progressive brain volume changes in schizophrenia are thought to be due principally to the disease. However, recent animal studies indicate that antipsychotics, the mainstay of treatment for schizophrenia patients, may also contribute to brain tissue volume decrement. Because antipsychotics are prescribed for long periods for schizophrenia patients and have increasingly widespread use in other psychiatric disorders, it is imperative to determine their long-term effects on the human brain.
Objective
To evaluate relative contributions of 4 potential predictors (illness duration, antipsychotic treatment, illness severity, and substance abuse) of brain volume change.
Patients
Two hundred eleven patients with schizophrenia who underwent repeated neuroimaging beginning soon after illness onset, yielding a total of 674 high-resolution magnetic resonance scans. On average, each patient had 3 scans (≥2 and as many as 5) over 7.2 years (up to 14 years).
Main Outcome Measure
Brain volumes.
Results
- During longitudinal follow-up, antipsychotic treatment reflected national prescribing practices in 1991 through 2009.
- Longer follow-up correlated with smaller brain tissue volumes and larger cerebrospinal fluid volumes.
- Greater intensity of antipsychotic treatment was associated with indicators of generalized and specific brain tissue reduction after controlling for effects of the other 3 predictors.
- More antipsychotic treatment was associated with smaller gray matter volumes.
- Progressive decrement in white matter volume was most evident among patients who received more antipsychotic treatment.
- Illness severity had relatively modest correlations with tissue volume reduction, and alcohol/illicit drug misuse had no significant associations when effects of the other variables were adjusted.
Conclusions
Viewed together with data from animal studies, our study suggests that antipsychotics have a subtle but measurable influence on brain tissue loss over time, suggesting the importance of careful risk-benefit review of dosage and duration of treatment as well as their off-label use.
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
Post-12:
We conducted a systematic review/meta-analysis of randomized trials, lasting 6 months comparing SGAs with FGAs in schizophrenia.
Primary outcome was study-defined relapse; secondary outcomes included relapse at 3, 6 and 12 months; treatment failure; hospitalization; and dropout owing to any cause, non-adherence and intolerability.
Across 23 studies (n=4504, mean duration=61.9±22.4 weeks), none of the individual SGAs outperformed FGAs (mainly haloperidol) regarding study-defined relapse, except for isolated, single trial-based superiority, and except for risperidone's superiority at 3 and 6 months when requiring ≥3 trials.
Grouped together, however, SGAs prevented relapse more than FGAs (29.0 versus 37.5%, RR=0.80, CI: 0.70-0.91, P=0.0007, I(2)=37%; NNT=17, CI: 10-50, P=0.003).
SGAs were also superior regarding relapse at 3, 6 and 12 months (P=0.04, P<0.0001, P=0.0001), treatment failure (P=0.003) and hospitalization (P=0.004).
SGAs showed trend-level superiority for dropout owing to intolerability (P=0.05).
Superiority of SGAs regarding relapse was modest (NNT=17), but confirmed in double-blind trials, first- and multi-episode patients, using preferentially or exclusively raw or estimated relapse rates, and for different haloperidol equivalent comparator doses.
There was no significant heterogeneity or publication bias.
The relevance of the somewhat greater efficacy of SGAs over FGAs on several key outcomes depends on whether SGAs form a meaningful group and whether mid- or low-potency FGAs differ from haloperidol. Regardless, treatment selection needs to be individualized considering patient- and medication-related factors.
Read the full article here:- http://www.nature.com/mp/journal/vaop/ncurrent/full/mp2011143a.html

Relapse prevention in schizophrenia: a systematic review and meta-analysis of second-generation antipsychotics versus first-generation antipsychotics
We conducted a systematic review/meta-analysis of randomized trials, lasting 6 months comparing SGAs with FGAs in schizophrenia.
Primary outcome was study-defined relapse; secondary outcomes included relapse at 3, 6 and 12 months; treatment failure; hospitalization; and dropout owing to any cause, non-adherence and intolerability.
Across 23 studies (n=4504, mean duration=61.9±22.4 weeks), none of the individual SGAs outperformed FGAs (mainly haloperidol) regarding study-defined relapse, except for isolated, single trial-based superiority, and except for risperidone's superiority at 3 and 6 months when requiring ≥3 trials.
Grouped together, however, SGAs prevented relapse more than FGAs (29.0 versus 37.5%, RR=0.80, CI: 0.70-0.91, P=0.0007, I(2)=37%; NNT=17, CI: 10-50, P=0.003).
SGAs were also superior regarding relapse at 3, 6 and 12 months (P=0.04, P<0.0001, P=0.0001), treatment failure (P=0.003) and hospitalization (P=0.004).
SGAs showed trend-level superiority for dropout owing to intolerability (P=0.05).
Superiority of SGAs regarding relapse was modest (NNT=17), but confirmed in double-blind trials, first- and multi-episode patients, using preferentially or exclusively raw or estimated relapse rates, and for different haloperidol equivalent comparator doses.
There was no significant heterogeneity or publication bias.
The relevance of the somewhat greater efficacy of SGAs over FGAs on several key outcomes depends on whether SGAs form a meaningful group and whether mid- or low-potency FGAs differ from haloperidol. Regardless, treatment selection needs to be individualized considering patient- and medication-related factors.
Read the full article here:- http://www.nature.com/mp/journal/vaop/ncurrent/full/mp2011143a.html

 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
Post-13:
- Occurs at age 12 years or younger and is often chronic and persistently debilitating
- According to the fourth edition of the DSM (DSM-IV), the criteria for childhood-onset schizophrenia and adult schizophrenia are synonymous, except for one potential modification for children (ie, in childhood-onset schizophrenia, the failure to meet expected social or academic milestones may be present, rather than deterioration in functioning).
- With the text revision of the DSM-IV (DSM-IV-TR), the criterion of social/occupational dysfunction in childhood or adolescent-onset schizophrenia can consist of a failure to achieve an expected level of interpersonal, academic, or occupational achievement.
- The prognosis for childhood-onset schizophrenia and adolescent-onset schizophrenia is worse than that observed in adult-onset schizophrenia.
- Patients with an onset before adolescence and those with an insidious onset appear to have a worse response to medication and a worse prognosis
- One half of these children have received previous diagnoses, including pervasive developmental disorders (PDDs), attention deficit hyperactivity disorder (ADHD), and internalizing disorders (eg, bipolar disorder, depression, anxiety disorders). In one study, psychotic symptoms appeared, on average, 2.5 years after the initial clinical presentation, and the diagnosis of schizophrenia was made a mean of 2 years after the onset of psychosis.
- Hallucinations (auditory more common than visual) are usually the presenting symptom and are reported by approximately 80% of children who receive the diagnosis of schizophrenia.
- Delusions are present in approximately 60% of patients.
- Ballageer et al found that bizarre behavior and negative symptoms were more common in individuals with adolescent-onset schizophrenia compared with those with onset during the adult years
- Compared with adults with schizophrenia, children with schizophrenia have catatonia less often
Childhood Onset Schizophrenia- HY Facts
- Occurs at age 12 years or younger and is often chronic and persistently debilitating
- According to the fourth edition of the DSM (DSM-IV), the criteria for childhood-onset schizophrenia and adult schizophrenia are synonymous, except for one potential modification for children (ie, in childhood-onset schizophrenia, the failure to meet expected social or academic milestones may be present, rather than deterioration in functioning).
- With the text revision of the DSM-IV (DSM-IV-TR), the criterion of social/occupational dysfunction in childhood or adolescent-onset schizophrenia can consist of a failure to achieve an expected level of interpersonal, academic, or occupational achievement.
- The prognosis for childhood-onset schizophrenia and adolescent-onset schizophrenia is worse than that observed in adult-onset schizophrenia.
- Patients with an onset before adolescence and those with an insidious onset appear to have a worse response to medication and a worse prognosis
- One half of these children have received previous diagnoses, including pervasive developmental disorders (PDDs), attention deficit hyperactivity disorder (ADHD), and internalizing disorders (eg, bipolar disorder, depression, anxiety disorders). In one study, psychotic symptoms appeared, on average, 2.5 years after the initial clinical presentation, and the diagnosis of schizophrenia was made a mean of 2 years after the onset of psychosis.
- Hallucinations (auditory more common than visual) are usually the presenting symptom and are reported by approximately 80% of children who receive the diagnosis of schizophrenia.
- Delusions are present in approximately 60% of patients.
- Ballageer et al found that bizarre behavior and negative symptoms were more common in individuals with adolescent-onset schizophrenia compared with those with onset during the adult years
- Compared with adults with schizophrenia, children with schizophrenia have catatonia less often
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
Post-14:

This video illustrates several forms of Catatonia including:
- Waxy flexibility,
- Forced grasping,
- Opposition,
- Negativism and
- Aversion.
This is intended to provide open access to teaching materials which, whilst originally designed for medical students, are hopefully of use for everyone interested in learning about psychiatry. It derives from the Newcastle University course and teaching resource.
Catatonia is a syndrome of psychological and motorological disturbances.
Karl Ludwig Kahlbaum first described it in 1874: Die Katatonie oder das Spannungirresein (Catatonia or Tension Insanity).
In the current Diagnostic and Statistical Manual of Mental Disorders published by the American Psychiatric Association (DSM-IV) it is not recognized as a separate disorder, but is associated with psychiatric conditions such as schizophrenia (catatonic type), bipolar disorder, post-traumatic stress disorder, depression and other mental disorders, as well as drug abuse or overdose (or both).
It may also be seen in many medical disorders including infections (such as encephalitis), autoimmune disorders, focal neurologic lesions (including strokes), metabolic disturbances and abrupt or overly rapid benzodiazepine withdrawal. It can be an adverse reaction to prescribed medication. It bears similarity to conditions such as encephalitis lethargica and neuroleptic malignant syndrome.
There are a variety of treatments available; benzodiazepines are a first-line treatment strategy. Electro-convulsive therapy is also sometimes used. There is growing evidence for the effectiveness of NMDA antagonists for benzodiazepine resistant catatonia. Antipsychotics are sometimes employed but require caution as they can worsen symptoms and have serious adverse effects.

This video illustrates several forms of Catatonia including:
- Waxy flexibility,
- Forced grasping,
- Opposition,
- Negativism and
- Aversion.
This is intended to provide open access to teaching materials which, whilst originally designed for medical students, are hopefully of use for everyone interested in learning about psychiatry. It derives from the Newcastle University course and teaching resource.
Catatonia is a syndrome of psychological and motorological disturbances.
Karl Ludwig Kahlbaum first described it in 1874: Die Katatonie oder das Spannungirresein (Catatonia or Tension Insanity).
In the current Diagnostic and Statistical Manual of Mental Disorders published by the American Psychiatric Association (DSM-IV) it is not recognized as a separate disorder, but is associated with psychiatric conditions such as schizophrenia (catatonic type), bipolar disorder, post-traumatic stress disorder, depression and other mental disorders, as well as drug abuse or overdose (or both).
It may also be seen in many medical disorders including infections (such as encephalitis), autoimmune disorders, focal neurologic lesions (including strokes), metabolic disturbances and abrupt or overly rapid benzodiazepine withdrawal. It can be an adverse reaction to prescribed medication. It bears similarity to conditions such as encephalitis lethargica and neuroleptic malignant syndrome.
There are a variety of treatments available; benzodiazepines are a first-line treatment strategy. Electro-convulsive therapy is also sometimes used. There is growing evidence for the effectiveness of NMDA antagonists for benzodiazepine resistant catatonia. Antipsychotics are sometimes employed but require caution as they can worsen symptoms and have serious adverse effects.
 Polypharmacy With Antipsychotics, Antidepressants, or Benzodiazepines and Mortality in Schizophrenia
Polypharmacy With Antipsychotics, Antidepressants, or Benzodiazepines and Mortality in Schizophrenia
Post-15:

Objective:
To investigate if the use of benzodiazepines, antidepressants, or multiple concomitant antipsychotics is associated with increased mortality among patients with schizophrenia.
Patients:
We linked national databases of mortality and medication prescriptions among a complete nationwide cohort of 2588 patients hospitalized in Finland for the first time with a diagnosis of schizophrenia between January 1, 2000, and December 31, 2007.
Main Outcome Measures:
Hazard ratios (HRs) were computed for all-cause mortality during the use of antipsychotics, antidepressants, or benzodiazepines in outpatient care, adjusting for the effects of sociodemographic and clinical variables, geographic location, and current and past pharmacological treatments.
Results:
- Compared with antipsychotic monotherapy, concomitant use of 2 or more antipsychotics was not associated with increased mortality (HR, 0.86; 95% CI, 0.51-1.44).
- Similarly, antidepressant use was not associated with a higher risk for mortality (HR, 0.57; 95% CI, 0.28-1.16) and was associated with markedly decreased suicide deaths (HR, 0.15; 95% CI, 0.03-0.77).
- However, benzodiazepine use was associated with a substantial increase in mortality (HR, 1.91; 95% CI, 1.13-3.22), and this was attributable to suicidal deaths (HR, 3.83; 95% CI, 1.45-10.12) and to nonsuicidal deaths (HR, 1.60; 95% CI, 0.86-2.97).
- In total, 826 of 904 patients (91.4%) who used benzodiazepines had purchased prescriptions that contained more than 28 defined daily doses, violating treatment guidelines.
Conclusions:
- Benzodiazepine use was associated with a marked increase in mortality among patients with schizophrenia, whereas the use of an antidepressant or several concomitant antipsychotics was not.
- Antidepressant use was associated with decreased suicide deaths.
- The literature indicates that long-term use of benzodiazepines among patients with schizophrenia is more prevalent in other countries (eg, the United States) compared with Finland, which suggests that benzodiazepine use may contribute to mortality among this patient population worldwide.
Source: Arch Gen Psychiatry. 2012;69(5):476-483
Polypharmacy With Antipsychotics, Antidepressants, or Benzodiazepines and Mortality in Schizophrenia
May 2012: Arch Gen Psychiatry. 2012;69(5):476-483.
May 2012: Arch Gen Psychiatry. 2012;69(5):476-483.

Objective:
To investigate if the use of benzodiazepines, antidepressants, or multiple concomitant antipsychotics is associated with increased mortality among patients with schizophrenia.
Patients:
We linked national databases of mortality and medication prescriptions among a complete nationwide cohort of 2588 patients hospitalized in Finland for the first time with a diagnosis of schizophrenia between January 1, 2000, and December 31, 2007.
Main Outcome Measures:
Hazard ratios (HRs) were computed for all-cause mortality during the use of antipsychotics, antidepressants, or benzodiazepines in outpatient care, adjusting for the effects of sociodemographic and clinical variables, geographic location, and current and past pharmacological treatments.
Results:
- Compared with antipsychotic monotherapy, concomitant use of 2 or more antipsychotics was not associated with increased mortality (HR, 0.86; 95% CI, 0.51-1.44).
- Similarly, antidepressant use was not associated with a higher risk for mortality (HR, 0.57; 95% CI, 0.28-1.16) and was associated with markedly decreased suicide deaths (HR, 0.15; 95% CI, 0.03-0.77).
- However, benzodiazepine use was associated with a substantial increase in mortality (HR, 1.91; 95% CI, 1.13-3.22), and this was attributable to suicidal deaths (HR, 3.83; 95% CI, 1.45-10.12) and to nonsuicidal deaths (HR, 1.60; 95% CI, 0.86-2.97).
- In total, 826 of 904 patients (91.4%) who used benzodiazepines had purchased prescriptions that contained more than 28 defined daily doses, violating treatment guidelines.
Conclusions:
- Benzodiazepine use was associated with a marked increase in mortality among patients with schizophrenia, whereas the use of an antidepressant or several concomitant antipsychotics was not.
- Antidepressant use was associated with decreased suicide deaths.
- The literature indicates that long-term use of benzodiazepines among patients with schizophrenia is more prevalent in other countries (eg, the United States) compared with Finland, which suggests that benzodiazepine use may contribute to mortality among this patient population worldwide.
Source: Arch Gen Psychiatry. 2012;69(5):476-483
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
Post 16-
Study: J Clin Psychopharmacol. 1986 Feb;6(1 Suppl):20S-23S.
Dosage strategies with long-acting injectable neuroleptics, including haloperidol decanoate.
First objective is to find the minimal effective dose for a given patient. It is advisable to give a trial of oral dosage prior to starting the decanoate form.
Initial monthly dose of haloperidol decanoate can be calculated using a decanoate to oral haloperidol equivalanet ratio of 10-15:1.
The steady state haloperidol concentrations are usually achieved by third or fourth dose of haloperidol decanoate given once every 4 weeks.
Study: Am J Psychiatry. 2002 Apr;159(4):554-60.
A Multidose Study of Haloperidol Decanoate in the Maintenance Treatment of Schizophrenia
OBJECTIVE:
Maintenance medication is critical in the prevention of psychotic relapse and rehospitalization among patients with schizophrenia. Given potential adverse effects, identification of the minimum effective dose is clinically important.
Advantages of Depot preparations:
- If a patient relapses, it is clear that the patient is relapsing despite medication, since injections have been given regularly.
- The correlation between the dose administered and the blood level obtained is significantly higher with depot than with orally administered medication
METHOD:
A multicenter, double-blind study was conducted to determine rates of symptomatic exacerbation and adverse effects in 105 outpatients with schizophrenia randomly assigned to four different fixed doses of haloperidol decanoate and treated for 1 year or until relapse. The doses used were 25, 50, 100, and 200 mg given intramuscularly once per month.
RESULTS:
- Rates of symptomatic exacerbation were 15% in the 200-mg group, 23% with 100 mg, 25% with 50 mg, and 60% with 25 mg.
- No significant differences in outcome were found between the groups treated with 200, 100, and 50 mg.
- Among the patients who completed the trial with no symptomatic exacerbation, there were no differences between dose groups on measures of psychopathology at the final rating point.
- The association between increasing haloperidol dose and increasing probability of not relapsing remained statistically significant when number of previous hospitalizations was used as a covariate.
- There were significant effects of dose on the analyses of covariance (ANCOVAs) at endpoint
(i.e., final ratings available for all patients, including those experiencing exacerbations) for the BPRS thought disturbance factor score, the total BPRS score, and the CGI severity and change scores. The patients receiving the lowest dose scored higher than those receiving the larger doses.
- Higher baseline scores on the BPRS thought disorder factor were correlated with relapse
- There were no significant differences in the use of antiparkinsonian medication, measured as either the proportion of time in the study that a subject received antiparkinsonian medication or the mean daily dose of anticholinergic medication administered
CONCLUSIONS:
- The results of this study suggest that the 200-mg/month dose of haloperidol decanoate is associated with the lowest rate of symptomatic exacerbation (15%) with minimal increased risk of adverse effects or subjective discomfort in comparison to 100 or 50 mg.
- At the same time, the rates of worsening with 100 mg (23%) and 50 mg (25%) were not significantly greater than that seen with 200 mg.
- These results provide some guidance as to effective dose ranges of haloperidol decanoate.
- On the basis of these data, dose reduction is difficult to justify, but the longer-term implications cannot be addressed with the current design. Without long-term data and a larger group of subjects it is difficult to draw conclusions regarding relative risk for tardive dyskinesia.
Study: J Clin Psychiatry 1992; 53:426–433
Depot neuroleptic therapy: an underutilized treatment option.
The risk of developing extrapyramidal side effects with fluphenazine decanoate is one and a half times as high as that associated with oral neuroleptics, whereas with haloperidol decanoate the risk appears to be 25% less than in comparison groups taking oral forms.

Haldol Decanoate- Dosing Strategies
Study: J Clin Psychopharmacol. 1986 Feb;6(1 Suppl):20S-23S.
Dosage strategies with long-acting injectable neuroleptics, including haloperidol decanoate.
First objective is to find the minimal effective dose for a given patient. It is advisable to give a trial of oral dosage prior to starting the decanoate form.
Initial monthly dose of haloperidol decanoate can be calculated using a decanoate to oral haloperidol equivalanet ratio of 10-15:1.
The steady state haloperidol concentrations are usually achieved by third or fourth dose of haloperidol decanoate given once every 4 weeks.
Study: Am J Psychiatry. 2002 Apr;159(4):554-60.
A Multidose Study of Haloperidol Decanoate in the Maintenance Treatment of Schizophrenia
OBJECTIVE:
Maintenance medication is critical in the prevention of psychotic relapse and rehospitalization among patients with schizophrenia. Given potential adverse effects, identification of the minimum effective dose is clinically important.
Advantages of Depot preparations:
- If a patient relapses, it is clear that the patient is relapsing despite medication, since injections have been given regularly.
- The correlation between the dose administered and the blood level obtained is significantly higher with depot than with orally administered medication
METHOD:
A multicenter, double-blind study was conducted to determine rates of symptomatic exacerbation and adverse effects in 105 outpatients with schizophrenia randomly assigned to four different fixed doses of haloperidol decanoate and treated for 1 year or until relapse. The doses used were 25, 50, 100, and 200 mg given intramuscularly once per month.
RESULTS:
- Rates of symptomatic exacerbation were 15% in the 200-mg group, 23% with 100 mg, 25% with 50 mg, and 60% with 25 mg.
- No significant differences in outcome were found between the groups treated with 200, 100, and 50 mg.
- Among the patients who completed the trial with no symptomatic exacerbation, there were no differences between dose groups on measures of psychopathology at the final rating point.
- The association between increasing haloperidol dose and increasing probability of not relapsing remained statistically significant when number of previous hospitalizations was used as a covariate.
- There were significant effects of dose on the analyses of covariance (ANCOVAs) at endpoint
(i.e., final ratings available for all patients, including those experiencing exacerbations) for the BPRS thought disturbance factor score, the total BPRS score, and the CGI severity and change scores. The patients receiving the lowest dose scored higher than those receiving the larger doses.
- Higher baseline scores on the BPRS thought disorder factor were correlated with relapse
- There were no significant differences in the use of antiparkinsonian medication, measured as either the proportion of time in the study that a subject received antiparkinsonian medication or the mean daily dose of anticholinergic medication administered
CONCLUSIONS:
- The results of this study suggest that the 200-mg/month dose of haloperidol decanoate is associated with the lowest rate of symptomatic exacerbation (15%) with minimal increased risk of adverse effects or subjective discomfort in comparison to 100 or 50 mg.
- At the same time, the rates of worsening with 100 mg (23%) and 50 mg (25%) were not significantly greater than that seen with 200 mg.
- These results provide some guidance as to effective dose ranges of haloperidol decanoate.
- On the basis of these data, dose reduction is difficult to justify, but the longer-term implications cannot be addressed with the current design. Without long-term data and a larger group of subjects it is difficult to draw conclusions regarding relative risk for tardive dyskinesia.
Study: J Clin Psychiatry 1992; 53:426–433
Depot neuroleptic therapy: an underutilized treatment option.
The risk of developing extrapyramidal side effects with fluphenazine decanoate is one and a half times as high as that associated with oral neuroleptics, whereas with haloperidol decanoate the risk appears to be 25% less than in comparison groups taking oral forms.

 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
Post-17
Abnormal Involuntary Movement Scale (AIMS)
CODE:
0 = None
1 = Minimal, may be extreme normal
2 = Mild
3 = Moderate
4 - Severe
MOVEMENT RATINGS: Rate highest severity observed. Rate movements that occur upon activation one less than those observed spontaneously.
Video Explanation of Abnormal Involuntary Movement Scale (AIMS):
0 = None
1 = Minimal, may be extreme normal
2 = Mild
3 = Moderate
4 - Severe
MOVEMENT RATINGS: Rate highest severity observed. Rate movements that occur upon activation one less than those observed spontaneously.
| Facial and Oral Movements | 1. Muscles of Facial Expression e.g. movements of forehead, eyebrows periorbital area, cheeks, including frowning blinking, smiling, grimacing | 0 1 2 3 4 |
| 2. Lips and Perioral Area e.g., puckering, pouting, smacking | 0 1 2 3 4 | |
| 3. Jaw e.g. biting, clenching, chewing, mouth opening, lateral movement | 0 1 2 3 4 | |
| 4. Tongue Rate only increases in movement both in and out of mouth. NOT inability to sustain movement. Darting in and out of mouth. | 0 1 2 3 4 | |
| Extremity Movements | 5. Upper (arms, wrists,, hands, fingers) Include choreic movements (i.e., rapid, objectively purposeless, irregular, spontaneous) athetoid movements (i.e., slow, irregular, complex, serpentine). DO NOT INCLUDE TREMOR (i.e., repetitive, regular, rhythmic) | 0 1 2 3 4 |
| 6. Lower (legs, knees, ankles, toes) e.g., lateral knee movement, foot tapping, heel dropping, foot squirming, inversion and eversion of foot. | 0 1 2 3 4 | |
| Trunk Movements | 7. Neck, shoulders, hips e.g., rocking, twisting, squirming, pelvic gyrations | 0 1 2 3 4 |
| Global Judgments | 8. Severity of abnormal movements overall | 0 1 2 3 4 |
| 9. Incapacitation due to abnormal movements | 0 1 2 3 4 | |
| 10. Patient’s awareness of abnormal movements. Rate only patient’s report No awareness 0 Aware, no distress 1 Aware, mild distress 2 Aware, moderate distress 3 Aware, severe distress 4 | 0 1 2 3 4 | |
| Dental Status | 11. Current problems with teeth and/or dentures | No Yes |
| 12. Are dentures usually worn? | No Yes | |
| 13. Edentia? | No Yes | |
| 14. Do movements disappear in sleep? | No Yes |
Video Explanation of Abnormal Involuntary Movement Scale (AIMS):
 Re: Schizophrenia- In Depth Explanation & Discussion
Re: Schizophrenia- In Depth Explanation & Discussion
POST 18:

Objective:
This study compares 3 cohorts of patients with schizophrenia before, during, and after initiating treatment with fluphenazine decanoate (FD), haloperidol decanoate (HD), or long-acting injectable risperidone (LAR).
Methods:
Administrative data are analyzed from California Medicaid (Medi-Cal) beneficiaries with schizophrenia who initiated FD, HD, or LAR treatment. Patients were required to have been continuously enrolled in Medi-Cal for 180 days before and 180 days after the start of the new episode of long-acting antipsychotic therapy.
Results:
- There were few demographic and clinical differences among patients initiating FD, HD, and LAR.
- During the 180 days before starting long-acting injections, most patients initiating FD (53.5%), HD (58.5%), and LAR (61.2%) received oral antipsychotic medications for <80% of the days in this period (medication possession ratio: <0.80).
- The mean duration of depot treatment episodes was 58.3 days (SD = 53.6) for FD, 71.7 days (SD = 56.4) for HD, and 60.6 days (SD = 48.8 ) for LAR (F = 18.3, df = 2, 2694, P < .0001, HD > FD).
- Few patients who started on FD (5.4%), HD (9.7%), or LAR (2.6%) continued for at least 180 days.
- Most patients in each group (FD [77.4%], HD [78.9%], and LAR [75.5%]) received oral antipsychotic medications during the 45 days after discontinuing long-acting injections.
- Coprescription with antidepressants, mood stabilizers, and benzodiazepines was common.
Conclusions:
- Patients treated with long-acting antipsychotic injections tend to have complex pharmacological regimens and recent medication nonadherence.
- A great majority of patients initiating long-acting antipsychotic medications discontinue use within the first few months of treatment.
Treatment of Schizophrenia With Long-Acting Fluphenazine, Haloperidol, or Risperidone
Schizophr Bull (2007) 33 (6): 1379-1387.
Schizophr Bull (2007) 33 (6): 1379-1387.

Objective:
This study compares 3 cohorts of patients with schizophrenia before, during, and after initiating treatment with fluphenazine decanoate (FD), haloperidol decanoate (HD), or long-acting injectable risperidone (LAR).
Methods:
Administrative data are analyzed from California Medicaid (Medi-Cal) beneficiaries with schizophrenia who initiated FD, HD, or LAR treatment. Patients were required to have been continuously enrolled in Medi-Cal for 180 days before and 180 days after the start of the new episode of long-acting antipsychotic therapy.
Results:
- There were few demographic and clinical differences among patients initiating FD, HD, and LAR.
- During the 180 days before starting long-acting injections, most patients initiating FD (53.5%), HD (58.5%), and LAR (61.2%) received oral antipsychotic medications for <80% of the days in this period (medication possession ratio: <0.80).
- The mean duration of depot treatment episodes was 58.3 days (SD = 53.6) for FD, 71.7 days (SD = 56.4) for HD, and 60.6 days (SD = 48.8 ) for LAR (F = 18.3, df = 2, 2694, P < .0001, HD > FD).
- Few patients who started on FD (5.4%), HD (9.7%), or LAR (2.6%) continued for at least 180 days.
- Most patients in each group (FD [77.4%], HD [78.9%], and LAR [75.5%]) received oral antipsychotic medications during the 45 days after discontinuing long-acting injections.
- Coprescription with antidepressants, mood stabilizers, and benzodiazepines was common.
Conclusions:
- Patients treated with long-acting antipsychotic injections tend to have complex pharmacological regimens and recent medication nonadherence.
- A great majority of patients initiating long-acting antipsychotic medications discontinue use within the first few months of treatment.
 Similar topics
Similar topics» Delirium- In Depth Explanation
» ADHD: In-Depth Discussion.
» Schizophrenia Discussion Thread.
» DELIRIUM in depth
» Interesting Case for Discussion
» ADHD: In-Depth Discussion.
» Schizophrenia Discussion Thread.
» DELIRIUM in depth
» Interesting Case for Discussion
FORUM FOR PSYCHIATRY RESIDENTS :: Psychiatry :: Psychiatry-Neurology-Psychology discussion :: Psychiatry In Depth
Page 1 of 1
Permissions in this forum:
You cannot reply to topics in this forum

» L-Methylfolate: Who Will benefit
» Vitamins & Supplements in Clinical Practice.
» Imaging Biomarkers for Outcomes in Mild TBI
» Q.5 Clozapine Neutopenia
» Treating Disorders!
» Cortical Abnormalities in Adults & Adolescents with MDD
» Efficacy of Antipsychotics in Pediatric Acute Mania
» Obsessive Compulsive Disorder in Adults: Which Treatment is Better?